Summary
The RIS implementation checklist serves as a practical compass for hospitals, guiding them in the right direction to reduce system complexity. This is not just a software setup but also provides a balanced alignment to people, process and technology. Clear workflows, clean data migration, proper training and compliance readiness are the core pillars of the checklist. When every step is defined beforehand, then go-live is no longer a chaos. This subtly lowers checklist delays, errors, and resistance in high-volume, high-pressure Indian hospitals. In this blog I will discuss how creating an RIS implementation checklist for hospitals provides smoother operations, faster reports, and better patient care without creating any noise.
Introduction
When hospitals are swamped with paperwork, phone calls, and delayed reports in the corridors, RIS implementation does not appear to be an IT project. It becomes a silent revolution. RIS implementation is not just about installing software. it’s about a sequence of small but significant conclusions. Data migration readiness, workflow mapping, user training, HL7 integration, and compliance checks all together push the system towards success or failure. Hospitals usually focus on technology and underestimate process and people.
The RIS checklist fulfills this gap. A structured RIS checklist provides clarity to hospitals about which step comes first, which will move in parallel, and which delays are not affordable. Cloud migration RIS allows Radiologists, technicians, IT teams and administrators to communicate with each other in one single shared language. In India’s healthcare ecosystem, where patient volumes are high and compliance pressures are constant, RIS implementation without a checklist will not give you fruitful outcomes for long-term. Checklist is a roadmap that simplifies complexity. It makes the system practices proactive and agile. And build the mindset of fixing errors beforehand. Finally, a well-defined RIS implementation checklist conceals the technology while revealing the care. When a system works efficiently, naturally doctors bring their focus more on patient care.
Why RIS Checklists Really Matter
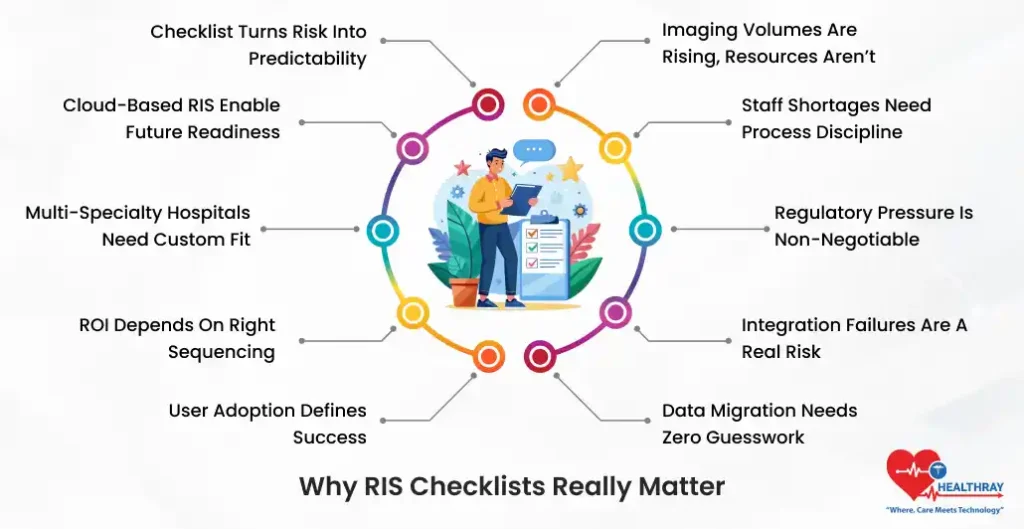
Imaging Volumes Are Rising, Resources Aren’t
The diagnostic demands in hospitals are increasing every year. However, radiologist and technician availability are not growing in parallel. Checklists provide a structure to workload.
Staff Shortages Need Process Discipline
Work is possible with limited staff only when the workload is standardized. Further, RIS software ensures automation and role clarity are settled beforehand.
Regulatory Pressure Is Non-Negotiable
Following standard HIPAA, NDHM (India) and the FHIR standard are not discretionary choices. It is highly imperative. In addition, the checklist brings the compliance from afterthought to the planning stage.
Integration Failures Are a Real Risk
Nearly 40% of RIS projects are struggling with HMS/EHR integration issues. Additionally, RIS cloud software prevents breakdown of checklist interfaces, HL7/FHIR mapping and validation.
Data Migration Needs Zero Guesswork
As we know, shift data from conventional system is extremely sensitive. Further, a structured checklist ensures completeness. Thus, helping clinics maintain precision and audit competence.
User Adoption Defines Success
Even the most powerful RIS can collapse if the user is not adequately trained. Further, checklists prioritize scenario-based training. And also provide go-live support upon completion of the deployment process.
ROI Depends on Right Sequencing
When clinics execute the implementation step in the appropriate direction, hospitals can accomplish measurable ROI in just 6 to 12 months.
Multi-Specialty Hospitals Need Custom Fit
Different departments follow different workflows. In this case a generic approach will not work out. Furthermore, the checklist makes the customization in-built and integral.
Cloud-Based RIS Enable Future Readiness
Cloud digital radiology workflow software such as Healthray ensures scalability and HMS/EHR integration in Indian and global markets.
Checklist Turns Risk into Predictability
In the end, a checklist is a control mechanism that converts uncertainties into structured progress.
Pre-Implementation Planning
Start with a Clear Needs Assessment
It is important to understand ground realities before RIS implementation. Next, thoroughly map existing scheduling delays, reporting turnaround issues, billing gaps and manual dependencies. Furthermore, accurate needs assessment is the right foundation for installation, more seamless adoption and future scalability.
Build a Cross-Functional Core Team
RIS implementation is not merely a radiology department project; it’s an organizational change. Radiologist brings clarity; IT specialists ensure system stability; administrators balance process and compliance; and the project manager keeps them in rhythm. Further, when roles are clearly defined through the RACI matrix, then ownership is completely transparent. Thus, the RIS checklist makes the decision fast ,minimise escalation and makes implementation a coordinated effort, not a tug of dispute.
Audit Infrastructure Before You Commit
Taking infrastructure too lightly is the biggest negligence clinics usually make before RIS implementation. It is crucial to objectively test bandwidth stability, server performance and PACS/HIS interoperability through HL7 and FHIR audits. Furthermore, Weak networks and incompatible interfaces seem invisible at the beginning. However, after going live, it becomes a silent reason for bottlenecks, downtime and user frustration. Moreover, a strong infrastructure provides certainty for future scalability and uninterrupted imaging workflows.
Set Realistic, Phased Timelines
RIS implementation is not a race; it’s a gradual process. Firstly, you should keep 2-4 weeks for planning the strategy to get clarity in every step of workflows. Secondly, keep 1-2 weeks for installation and technical stability. Next, keep 3-4 weeks for testing and real-world validation. Treat optimization as a continuous improvement. When timelines are realistic, errors are fewer and adoption is very smooth. Rushing the implantation is not a strategic move; it’s just like creating short-term gain and long-term pain.
Choose Vendors for Tomorrow, Not Just Today
RIS vendor selection should not be limited to solving only present problems. Further, AI algorithmic analysis, mobile accessibility, voice automation and conformity abilities are not fancy teams; they have become the basic expectation. Platforms like Healthray include built-in PACS and seamless integration. Also, healthray offers long-term scalability and an innovation roadmap. Always remember, a right vendor will convert the future disruption into a competitive advantage. Also, read our blog on the benefits of radiology management software to get interesting information about RIS.
Installation and Data Migration
Go Cloud to Cut Complexity
Installing cloud-based RIS is all about skipping heavy hardware expenses and maintenance headaches. Furthermore, configure auto-order routing for modalities like CT, MRI aur X-ray. This will help clinics eliminate manual handoffs.
Plan Data Migration Like a Mission-Critical Task
Taking legacy data lightly is the biggest risk. First, clinics should take full backups. Then map accurate fields among patient IDs, study numbers and DICOM headers. It is highly advisable to validate 100% data integrity.
Phase 1: Sandbox Setup (1 Week)
In this stage, test core RIS modules in an isolated environment. It helps clinicians fetch errors at this stage.
Phase 2: Pilot Migration (10% Data)
First, transmit the minimal data and pinpoint the variation. These small samples prevent large-scale failures in futures.
Avoid the Legacy Silo Trap
Conventional systems usually break the real-time synchronization. Solution is simple. Use FHIR bridges, which help clinics ensure continuous data flow.
Why Healthray Speeds Things Up
Healthary boasts plug-and-play architecture. Further, it minimizes migration time up to 70% through intelligent data mapping. Thus, causing less disruption and expediting stabilization.
Testing Protocols
Run End-to-End, Not Just Module Tests
Testing is not about checking buttons. Further, stimulate 500/orders for scheduling and billing. This will help radiologists understand radiology information behavior in real workloads.
Follow a Structured Testing Stack
A checklist should include unit testing (module-wise), integration testing (RIS–PACS/HIS), and UAT testing. One of the most important aspects of adoption is the involvement of radiologists in UAT.
Stress Test for the Worst Days
Test peak-hour loads and system failover or downtime scenarios. RIS systems that remain stable during pressure can survive in production.
Don’t Skip Security Audits
Penetration testing and role-based access ensure validation to keep the security and compliance requirements functional.
Track Clear, Measurable Metrics
It is highly imperative to set the targets: less than 2% error rate and 95% of orders less than 5 minutes for processing. Additionally, numbers display the honest answer. Relying just on opinions is not a productive move.
Use Clinical Champions for Feedback
Take feedback from power users and champions and iterate it. Repeat it unless you are able to achieve a 99% pass result.
Step towards digital era with our healthcare solution
Revamp your hospital facilities and embrace change for better healthcare management. Ease in managing and organizing large medical datasets leads to effective analysis. Seize the opportunity now!
Customizing RIS for Specialty Workflows
One-Size-Fits-All Doesn’t Work
Standard RIS templates are generally too small in the fields of mammography and interventional radiology. Therefore, it is crucial to tailor the modules as per hospital-dependent process requirements. This helps clinics discover real success.
Smart Hanging Protocols Save Time
Custom hanging protocols populate previous experiences and measurements. Thus, helping radiologists reduce reporting time for solving complex cases.
Voice-Enabled Macros Change Reporting Speed
Train AI so that phrases like “BIRADS 4 mass at 2 o’clock” instantly get converted to structured reports. Thus, eliminating the need for manual typing and simultaneously minimizing delays.
Mobile-First Tweaks for Modern Radiology
When performing ward rounds or traveling, radiologists can approve the concerns using smart devices like a phone or tablet. Furthermore, RIS software instantly connects with PACS, thus minimizing dependency on desktops.
Post-Implementation Optimization
Measure What Truly Matters
After go-live, don’t just assume the success. It is highly crucial to measure it as well. KPI studies such as a 30% increase, a 20% error reduction, and a 98% billing accuracy are the reflection of real performance.
Keep Upgrading, Don’t Freeze
Enhancement of AI-based auto-prioritization reduces backlog and TAT. Also, it slows down the static systems.
Scale with Centralized Control
For multi-site hospitals, centralized dashboards ensure consistency and visibility without losing local flexibility.
Use Analytics for Predictive Improvements
System analytics are not solely for reporting. Furthermore, predictive analytics alerts clinics about bottlenecks and uncertainties beforehand. Thus, helping clinics maintain stability and a smooth environment even in chaotic situations.
Conclusion
With the right RIS implementation, radiologists no longer just remain a support function; instead, it becomes an avenue for growth and income generation. Structured approach integration eliminates traditional problems of delays and user resistance. When RIS implementation checklists are properly aligned with the unique workflow of the hospital, then RIS can present a true competitive edge.