Summary
Recurring doctor appointment scheduling combines chronic care follow-ups into a single flow. Daily administrative tasks and follow-up management often make the process complicated. Especially in the case of chronic patients, missing regular appointments can directly impact treatment continuity. The best solution to circumvent this problem is recurring doctor appointment scheduling software. In this blog, I will discuss how recurring doctor appointment scheduling automates follow-ups so that doctors can focus on their core medical duties. Also, I will discuss how recurring scheduling ensures timely consultations for chronic care patients and makes the clinic’s daily operation smooth. Let’s begin!!!!
Introduction
One of the most difficult challenges confronting the healthcare industry today is effectively managing chronic patients with regular follow-ups, continuous monitoring, and timely consultations, which is highly imperative. Doctors and staff mostly encounter challenges with the manual tracking of recurring appointments, which results in missed visits, delayed treatments, and frustrated patients. In these busy clinical environments, traditional scheduling approaches no longer make sense. Adopting recurring doctor appointment scheduling is no longer merely an option to address this issue; it is now a necessary requirement for clinics.
This advanced doctor appointment system allows clinics to maintain a consistent follow-up rhythm while also ensuring that chronic care patients do not miss important appointments. Beyond that, it reduces administrative workloads and structures the doctor’s daily routine. Now you might be thinking, why is recurring scheduling software important for chronic patients? The simple answer is consistency and continuity of care. When follow-ups are auto-scheduled, patients feel more confident. and doctors get a clear view of treatment progress and care plans work smoothly without interruption.
Additionally, this advanced system improves chronic care delivery by improving patient adherence and reducing no-shows. Doctors can remotely access schedules, timely adjust their day-to-day routine and ensure patients get continuous and reliable care. Keep reading this article to know how recurring appointment scheduling makes chronic care management smarter and more effective.
Why Chronic Care Needs Recurring Follow-Ups
Chronic conditions such as diabetes, hypertension, COPD, heart failure, and kidney disease are not one-time treatments; they require long-term, planned monitoring where care does not depend on visits; instead, they depend on continuity.
Regular Follow-up Maintain Strong Care
With regular follow-ups, doctors can timely adjust the medicine, review the labs reports and consistently guide the patients for self-care management. Furthermore, these regular routine check-ins capture the health deterioration at an early stage. Thus, it naturally curbs unnecessary ER visits and hospital admissions.
Missed Follow-ups Negatively Impact Results
When follow-ups get missed or delayed, later on disease control becomes weak. Further, it increases complications, creates treatment gaps and silently raises the overall healthcare cost. Therefore, follow-up reliability is not just an operational task; instead, it’s a core indicator of chronic care quality.
The Cost of Missed and Late Appointments

Let’s dive in:
Real Cost of Missed and Late Appointments
In most outpatient clinics, no-show rates almost reach double digits, highlighting the importance of having a clear no-show policy. Additionally, the majority of patients with persistent symptoms frequently miss appointments. Also, transport issues, work pressure, and health literacy gaps make the care more fragile.
Every Missed Visit = One Lost Care Moment
Missed appointments result in more than just the slot becoming empty. Treatment plans fail to adjust in a timely manner, lab abnormalities go unnoticed, and early warning signs silently disappear. Further, in chronic care, these small delays eventually become a big complication for patients.
Silent Pressure on Clinic Operations
At the operational level, no-shows waste considerable time of doctors. Further, this impedes schedule templates and slows down the revenue realization. Also, it shifts the staff to reactive mode, where energy is utilized on urgent coordination rather than planned care.
Difficulties in Accessibility for High-Risk Patients
When missed appointments become a pattern, clinics are incapable of providing timely slots to patients that are genuinely struggling with high-risk symptoms and want instant care. Further, this gap breaks the care continuity and eventually weakens the patient’s trust.
What “Recurring Appointment Scheduling” Really Means
Recurring appointment scheduling is not about booking next visits. Furthermore, it is an unplanned approach, where chronic care patients’ follow-ups are already set in a predictable rhythm instead of last-minute coordination.
Think beyond a one-time reservation
In the doctor appointment calendar system model, patients no longer need discussion on next visits. As follow-ups have already been scheduled for next week or month. Thus, software ensures continuity of care and naturally avoids gaps.
Minimizes Mental Load on Patients
Patients no longer need to remember appointments or take the unnecessary stress of booking appointments for next check-ups. Now, for patients, care becomes a steady routine. This helps patients to maintain consistency with their chronic symptoms.
Predictable Flow for Clinics
Recurring scheduling software creates a stable calendar for clinics. Further, it efficiently balances the doctor workloads and eases staff coordination. It becomes easily manageable to provide timely access to high-risk patients.
Care Continuity Becomes Naturally Strong
When the cloud-based doctor booking system consistently repeats follow-ups, care no longer depends on patient memory. Overall, this reliability silently improves the chronic care quality. In the long run, patients get immense benefits, and they are capable of handling their chronic symptoms successfully.
Why “Set it and Forget it” Matters for Patients
Chronic care patients are already managing their medicines, diet, reports, and symptoms. The care burden also increases if they have to remember every single appointment. Let’s check out how the “Set it and forget it” approach minimizes this pressure:
Naturally Reduces Mental Burden
When follow-ups are pre-scheduled, then patients no longer have to call staff and invest in proper planning. As daily care becomes a predictable routine for chronic patients, doing this minimizes anxiety and improves adherence.
Care Does Not Depend on Memory; Instead, it Depends on the System
Sometimes a disruption in life causes a patient to forget appointments. Furthermore, when the doctors’ appointment system for modern healthcare automatically handles a follow-up, care continuity no longer hinges on the patient’s memory. This consistency is critical for chronic disease control.
Strong Signal of Trust and Safety
When clinics proactively manage appointments, patients feel their care is continuously under consideration. Further, this reassurance builds trust and consistently engages the patients, without any manual effort.
Patients feels more connected
The “set it and forget it” approach helps patients transition from receiving reactive care to feeling more centered. When patients feel valued, then they naturally complete follow-ups and make the outcome more satisfactory.
Building Blocks of a Recurring Scheduling Workflow
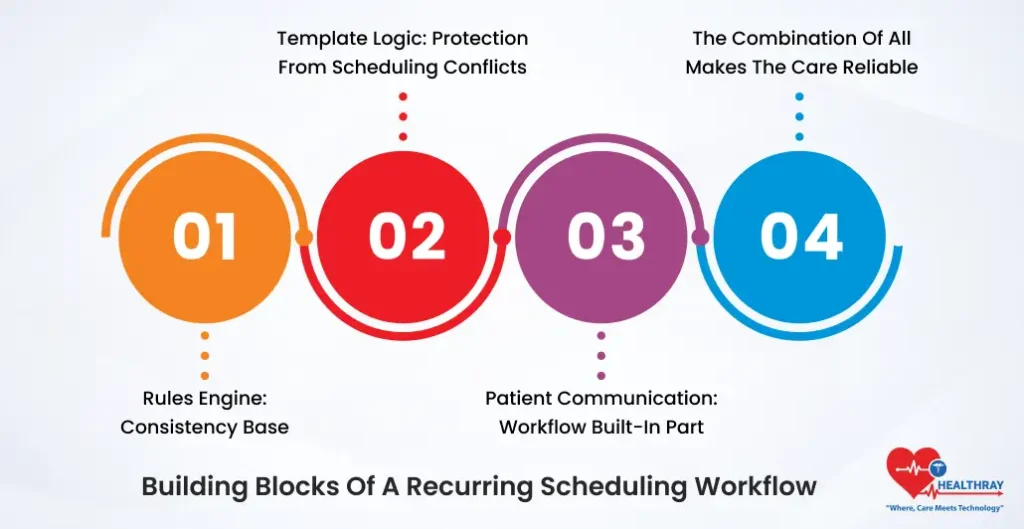
A strong recurring follow-up does not depend on single features. Further, it combines with multiple components and works efficiently and renders every step of healthcare predictable and reliable.
Rules Engine: Consistency Base
The initial block is the rules engine. Further, it defines default follow-up frequency as per conditions, such as 3-6 months for stable diabetics and 1-2 for uncontrolled cases. Thus, it allows the front desk and providers to follow the same pattern, without any ambiguity.
Template Logic: Protection from Scheduling Conflicts
Next comes the template logic. Here, appointment types, visit duration, and provider availability are already mapped. It automatically circumvents overbooking and schedule conflicts while establishing a schedule.
Patient Communication: Workflow Built-In Part
Next important block is patient communication. It seamlessly integrates with reminders, confirmations, and two-way messaging series. Patients no longer need to put in manual efforts on every visit. Also, patients remain consistently attentive about their next visits.
The Combination of All Makes the Care Reliable
When all the building blocks work together, recurring schedule software no longer remains an operational task. It becomes a dependable system for chronic care that minimizes pressure on both staff and patients.
Essential System Capabilities to Support Recurrence
Recurring schedules are not just bound to a single “repeat” button at the software level. System should be both flexible and intelligent to smoothly navigate the real clinic workflows.
Flexible Recurrence Patterns Support
System should support different recurrence patterns daily, weekly, monthly, and custom intervals. Also, the system should provide options for start date, end date, and setting up a fixed number of occurrences to align follow-up according to the care plan.
Smart Presets: Condition- or Provider-Based
Condition-based or provider-based presets are crucial for continuity and care. As a result, there is no longer a need to schedule each patient from the beginning. Also, the team follows the same protocols without spending time in extra coordination.
Override Control Without Breaking the Series
Clinics sometimes have to reschedule or cancel specific appointments. Further, a system should be capable enough to handle unexpected change and keep the entire series functional. This flexibility helps clinics handle real-world disruptions.
Automatic Protection from Overlapping Bookings
When schedules and providers change their roster, the system should be capable of preventing overlapping bookings. Further, these safeguards keep the clinic calendars neat and avoid last-minute havoc.
Care Alignment with EHR / EMR Integration
EHR, or EMR integration, ensures all the important parameters, such as correct visit type, reason, and documentation templates, are properly attached. This allows scheduling and clinical documentation to work in the same flow without any manual corrections.
Conclusion
Recurring, rule-driven scheduling software transforms chronic care from a reactive, visit-by-visit process to a continuous and proactive program. This is not just a convenience feature for clinics. It becomes an essential infrastructure layer for chronic care that protects revenue and supports team efficiency to ensure high-risk patients never fail to attend the appointments.





