Quick Summary: Patient enrollment, insurance verification, charge entry, claim submission, payment advertisement, rejection running, prayers, patient statements, follow-up, and reporting are the ten ways in medical billing process. These guarantee correct payment for medical services rendered.
Introduction
Medical billers and coders are fortunate to enjoy flexible work schedules since numerous enterprises allow them to work from home or in the office.
Medical billing and coding are becoming a popular career choice for many, as the healthcare industry continues to have a high demand for good individuals.
Since they validate the details of a case’s visit to medical practices and the insurance system, medical billers and coders are an essential element in determining the financial responsibility of the healthcare system.
You might want to learning more about how medical billing functions and how the healthcare institution, medical biller, insurance company, and medical system reuse a claim. The ten ways in the medical billing cycle are as below.
What is Medical Billing?

Medical billing is a method of payment in the US healthcare system. To get paid, the process involves filling out standard forms and submitting medical claims. Following the care provision, the healthcare professional thoroughly documents the case’s visit, including the opinion, treatments, and any traditional medicines given. Using the applicable coding system known as medical coding for converting data into standard canons. Along with the case’s insurance information and demographics, medical billing submits these enciphered records to the payer or the health insurance company. Whether for-profit businesses or government-patronized enterprises, the maturity of insurance companies follows an analogous procedure.
After reviewing the claim, the insurance provider confirms the case’s insurance plan- grounded content eligibility and medical necessity. In the event of claim approval, the insurance provider will either pay the medical professional directly or refund the case. It can be necessary for the healthcare provider to probe and challenge claims.
For the medical billing process to guarantee prompt and accurate payment for handed healthcare services, delicacy, familiarity with insurance programs, and understanding of coding conditions are necessary. Although it’s not reasonably mandatory, medical billers prompt to earn instruments by passing a test.
The thing about instrument programs is to give beginners to the medical billing industry a theoretical foundation. In the US, many community colleges offer associate’s degrees or instruments in the subject. One can earn a bachelor’s or graduate degree in medical information wisdom and technology if they want to facilitate through cross-training in medical coding, recap, or auditing.
Though it might ameliorate job chances, an instrument isn’t necessary to master billing, and state-by-state differences live in billing procedures.
10 steps involved in the medical billing process
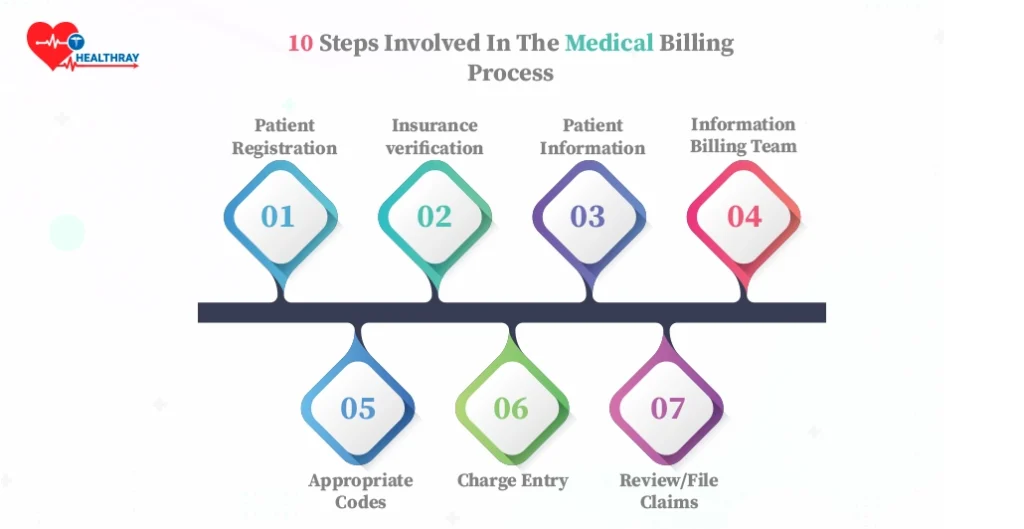
Patient Registration
Every visit, anyhow of how long a case has been seeing you, should start with some form of patient enrollment. A comprehensive medical history, including the patient’s demographic information and data, should be attained during the original discussion for record-keeping purposes.
Verify that all the material details are in the train, including the case’s address, phone number, insurance information, and so on, if they’re routine cases. Vindicating a date of birth, valid insurance card, or address will guarantee that all data is present in the correct case file.
Insurance verification
Verify that you have the case’s insurance information up to date and accurate during enrolment. You should also find out if any fresh visits bear billing, depending on the nature of the appointment( worker’s compensation, accident, etc.). Using Medical Billing Software can help you make the insurance process easier.
In this phase, you can confirm that the case or patient’s insurance coverage is over to date, that you have their accurate information, and that you have reviewed their out-of-pocket charges. Vindicating this information now will help help billing problems and detainment in the future.
Record Patient Information
Record all of the information bandied at the appointment during the visit. Take thorough notes or record the meeting( audio or videotape), if possible. A medical coder must review this information after the meeting to apply the proper canons to the visit.
After the visit, the meeting might be transcribed. Verify that the visit’s purpose is apparent, that any judgments are present, that the specifics are known, and so forth. It will benefit your billing and rendering staff and give your case a further comprehensive medical history for future reference.
Send Information to the Billing Team
After the appointment, the medical recap — also known as a medical script is understood and ready for the medical billing staff. However, if you do this internally, you can give your workers the tape recording to take notes and transcribe it. Verify the medical script for crimes if you sell through a third party.
It is a pivotal stage in the procedure and prone to crimes. Your coders, medical billers, and cases will appreciate how much easier it is if you’re clear, brief, and comprehensive when transcribing.
Apply Appropriate Codes
You or your coding platoon will determine whether CPT or HCPCS law is suitable for the services you rendered. Ensure the element services are not assessed collectively if they’re whisked with the primary procedure, and elect the law that most rightly reflects the work completed.
The step is to elect the applicable ICD-10 canons, either you or your coders, for the case’s judgments. Also, there are a ton of canons — roughly 68,000 — to elect from. There were nearly 13,000 canons available in the former edition(ICD-9), which is about five times as many canons to sort through! For this reason, the information you include in the case’s medical training is pivotal.
Charge Entry
Your billing team will now prepare the medical claim using the visit canons. Using the proper canons is pivotal because using the wrong one could significantly change the charges. Likewise, the freights aren’t standard, despite the canons being similar.
Ensure all costs are included in the list with the applicable visit canons. A well-defined list of medical services will help you minimize miscalculations and expedite the procedure. Any crimes made then could result in the insurer refusing to pay or repay you and your claims being denied. It may also impact the possible out-of-fund charges for your case.
Review/File Claims
You will have to file a claim for payment after they’ve been checked for delicacy. It can be electronically and frequently through two review processes: one for scrubbing and another for reviewing. The software guarantees that all form fields are met and that the associated canons and freights make sense.
After that, they deliver claims to a clearing house for a last examination. After doing a previous review of the fundamental data( name, current insurance checks, date of birth, etc.), they reformat the claim for each payer collectively( because not all payers follow the same format).
Insurance Adjudication
At this point, the insurance provider will reuse the claim, check whether the treatments or procedures are present, and either authorize or reject it. However, it will remove the claim; a thorough defense and instructions for fixing any problems will still be handed in if there are miscalculations. After that, you can resubmit the claim.
They might reject the claim sometimes because the insurance simply doesn’t cover the services. It is where the primary work pays off, particularly regarding the case’s insurance content. Realizing they do not have content when they allow doing terrible things to be right now.
Prepare Patient Statement
Preparing statements for your case, assuming all the information is correct. However, if the quantum isn’t zero, the charges and benefits they admit or don’t admit from the insurer should be made veritably clear. As a result, they get knowledge of the charges and their amount. Give information on how to make payments, deadlines, and how a case might dispute costs with their insurance.
Patient Follow Up/Payment
Entering payment from the case and the insurer completes the procedure. After approval of claims, payments to insurance companies are automatic. Patients may choose to prepay for a procedure or for a visit in advance (co-pay). Some people may choose to pay at unusually young ages.
Even though each process stage is pivotal, getting compensation for your services enables you to earn money, pay your workers, and maintain serviceability. You might have to go through collections, but you must meet deadlines with your cases before they start paying.
Get your medical billing software with Healthray!

You may simplify your healthcare business using Healthray’s cutting-edge medical billing software. We bid a happy farewell to handcrafted billing problems and welcomed effectiveness with our smart outcome. Improve your financial performance, cut down on errors in computations, and maximize your profit cycle. Healthray’s software meets the unique needs of medical practitioners while ensuring compliance with ever-changing regulations.
Profit from the real-time shadowing, the comprehensive reporting, and the ease of submitting claims.
Our wealth of features streamlines billing procedures so you can concentrate on giving patients the treatment they need. Use Healthray to compute for a dependable, secure, and reasonably priced medical billing solution. Our Medical Billing Software Solutions article can help you have more ideas. Get your Healthray today to start on the path to financial success in the healthcare sector!
Conclusion
Let’s review the main ideas as we come to the end of our blog post on the 10 ways in the Medical Billing Process. You can simplify your profit cycle operation, stay down from expensive crimes, and guarantee that your payment of services on time by following these guidelines. Every stage of the billing process, from patient enrollment to payment collection, is vital. So snare a seat, and learn these ways to maintain both patient satisfaction and a strong fiscal position for your practice!