Laboratory billing across the globe depends on a slender pillar of trust in the healthcare system and is often faced with challenges. From coding errors to claim rejections, these inefficiencies in the billing processes delay payments and create a financial crisis. These are the pain points that lab managers, healthcare administrators, and pathology managers look to find solutions for.
AI is marching in the great revolution of laboratory billing functions. Automating mundane tasks, identifying anomalies, and enhancing accuracy, AI is converting the billing process into one seamless activity. But how does AI really stand to make its magic work, and what does it mean for the laboratories and their managers?
Current Challenges Laboratory Billing

Laboratory billing is very important, indeed, but it has faced much interference with challenges to efficiently execute procedures and generate revenue. Below are some common challenges lab managers and healthcare administrators get confronted with.
Coding Errors and Billing Issues That Slow Down Operations
Different coding systems have great significance on laboratory billing, e.g., CPT and ICD codes, all of which must relate to the service provided. Apparently, even the minutest error needs to be avoided because it causes rejection or delay of the claims.
High Incidence of Claim Denials
Differences in patient information as compared to what is being submitted on the claim forms; loss of the paper trail or, in plain words, most times disregarding insurance regulations, are more circumspections for the administration, creating unreasonable delays in payment, bringing the cash flows further into disrepute.
Wasting Time With Administrative Duties
Bill generation is still largely manual for many of the laboratories where manual entries take so long, and with much error, that the entire laboratory billing process is bottlenecked, wasting both time and resources.
Galactic Complexity
Navigating an infinitely deep labyrinth of requirements, innumerable insurance companies with divergent policies, authorization requirements, and reimbursement terms remains the greatest and foremost challenge.
Real-Time Reporting-Hobgoblin
Normal systems are not real-time visible, with lab management incapable of recognizing trends and exceptions- contrary to the earlier discussed proactive approach.
Thus, these challenges firm up the necessity of smart systems being implemented to better streamline laboratory billing. Are you ready to see how AI can solve these challenges? Let’s get into it.
AI Solving Billing Problems

With its power, AI is walking its step, examining inefficiencies toward automation. But it’s not just building a system faster; it’s building intelligent systems that learn and improve. The following information shows how AI combats the most pressing billing challenges:
Reduction in Coding Errors-Billing Errors
With the help of AI, CPT and ICD codes are interpreted intelligently and compared with appropriate service record standards for billing purposes. With AI, one can continue to automate the coding process with these errors via an incorrect approach, thus rejecting more claims.
In addition, constant situation incidences will train machine-learning algorithms to give a user interactive experience that is dependable.
Magic Compliance Monitoring Tools
The evolution of regulations and AI systems keep laboratory files current with payer rules and statutory requirements, identifying potential compliance risks and shielding labs from fines or penalties.
These systems would also help labs save time and cost, thus allowing further involvement of the labs with patient care. Following that, we shall look into how the integration of these systems into the regular ones casts greater efficiency.
Integrating AI into Existing Systems for Billing
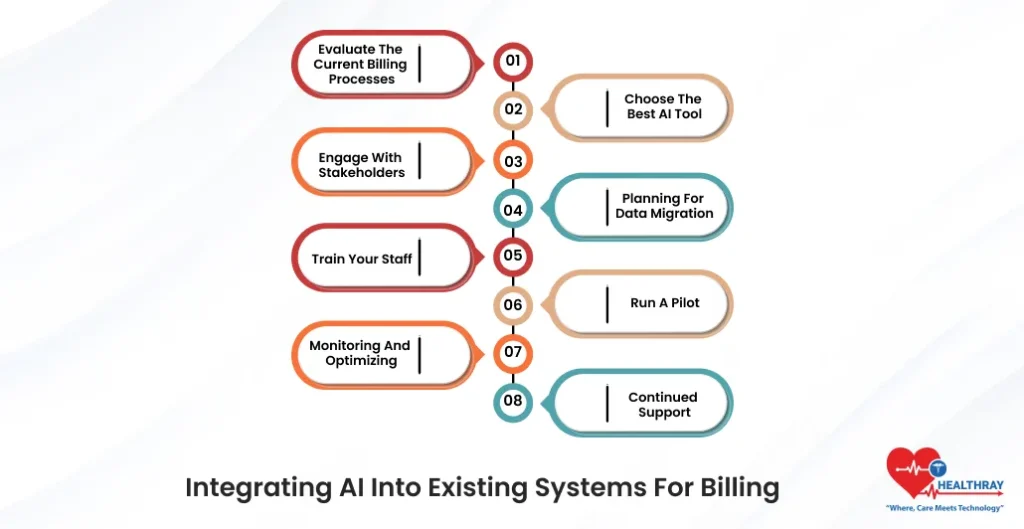
Installing an AI tool for lab billing is one matter; actually getting it to work is another, and an even bigger challenge is its fusion with-the-existing work view. Below is a brief step-by-step overview.
Evaluate the Current Billing Processes
Start by assessing any issues about current billing processes. Identify the existing bottlenecks caused by frequent errors, delays, or higher claim denials and how they can be solved with AI tools.
Choose The Best AI Tool
Choose an AI tool that meets the lab’s needs and budget. It should ideally come with features for automating coding, scrubbing claims, real-time analytics, and compliance tracking. The integration should work seamlessly with the existing EHR or billing software.
Engage With Stakeholders
Carry out engagement on the integration with as many stakeholders as possible, from laboratory management, billing, and IT. They would provide insight regarding any practical inconvenience and the design of the system to fit everybody.
Planning For Data Migration
The migration plan should include the secure and efficient transfer of data if your lab has an old billing system currently housing all data. Proper data is essential for the proper working of the AI tool; thus, the migration should be smooth.
Train Your Staff
Train all the staff before using AI tools on the new system. Training should touch on both the technical side and motivation, which will neutralize a considerable amount of initial reluctance in using the new system.
Run a Pilot
Before Full Deployment Before rolling it out, it is better to test the application on a smaller scale. This way, its performance can be kept under observation on a smaller base while tweaking any foul-ups.
Monitoring and Optimizing
Having fully implemented the AI tool, the next move is establishing a regular protocol for measuring its performance. AI tool insights will be used to inform adjustments going forward.
Continued Support
Establishing a partnership with the AI tool provider for continued support and updates is necessary. Regulations and billing requirements change over time, thus frequent patches ensure that your system is up to date and functional.
The upfront integration of AI into your billing system will stand you in good stead for these minor actions in the long run when there are fewer errors, faster payments, and streamlined workflow. Move on to see how AI impacts compliance and costs.
Compliance as well as Cost Considerations

Compliance with healthcare regulations and cost are the two critical considerations concerning AI applications in laboratory billing. Both compliance and cost are critical to successful deployment of AI tools. Let’s look at them individually.
Compliance with the Healthcare Regulations
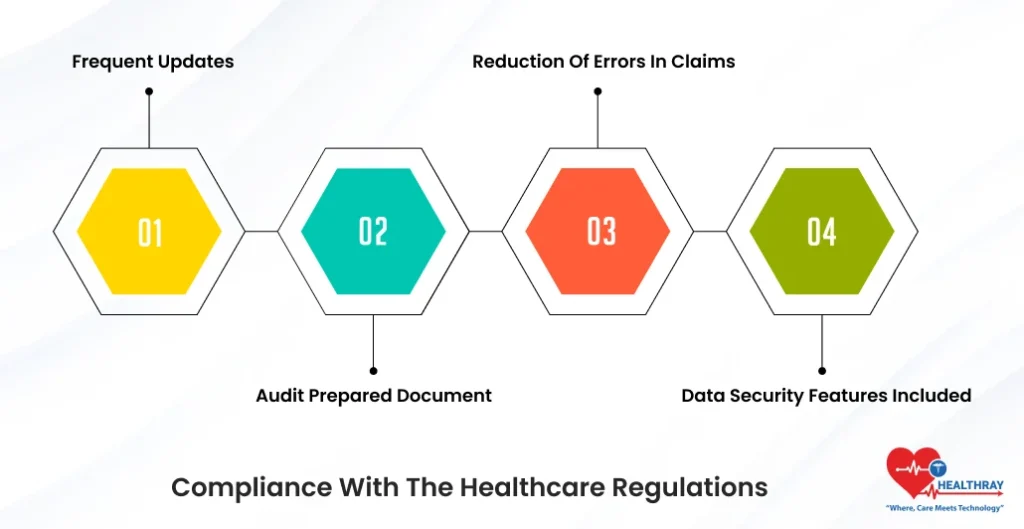
The AI-enabled billing tools have been built with compliance to industry regulations, such as the U.S.-based HIPAA (Health Insurance Portability and Accountability Act), to make safeguards around patients’ data and privacy. Here’s how AI addresses the compliance issues:
- Frequent Updates : AI being updated constantly with all new payer rules and changes in the regulations, hence reducing incidence errors from old practices.
- Audit Prepared Document: Documentation of billing activities very exhaustive and well organized by AI tools, which correspondingly makes it very easy for an audit and compliance preparation.
- Reduction of Errors in Claims: Automated processes in the creation through AI and hence less the penalties and/or fines that would have been incurred were found.
- Data Security Features Included: Almost all AI solutions come coupled with encryption, role-based access, and several other security measures.
Cost Assessment for AI Adoption
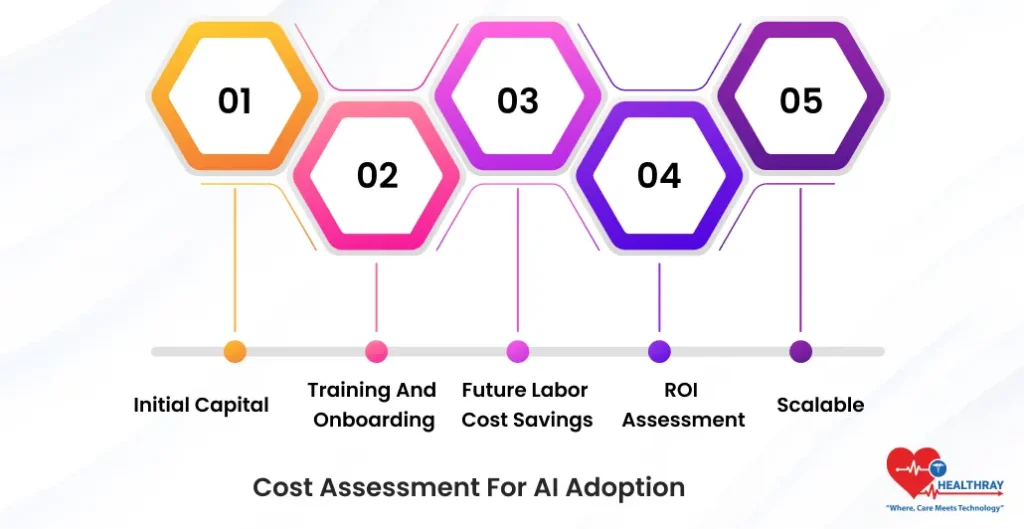
The most out of costs in implementation varies between factors, and AI billing solutions probably fetch from investments because they yield efficiencies in revenue cycles afterward. Cost evaluation should be measured against:
- Initial Capital: This covers acquisition of AI tools, installation, and data transfer. Acquisition costs will certainly be lower when using laboratory resource cloud solutions.
- Training and Onboarding: Training of workers is necessary and may need additional resources to smoothen adaptation to the new system.
- Future Labor Cost Savings: In the long run, AI will cut labor costs by automating repetitive tasks and reducing claims rejections thus speeding reimbursements with fewer write-offs.
- ROI Assessment: Incorporate revenues into ROI tracking through built-in analytics of AI for financial impact monitoring in collection metrics, including reduced denial rates and increased cash flow.
- Scalable: Choose solutions adaptable to the growth of your laboratory and require less frequent upgrades or replacements.
Tremendous benefits can be gained from adopting AI, but truly worth the investment, as it simplifies compliance while generating returns. The next section is going to show real examples of laboratories that have adopted AI in their billing processes. Do prompt me when ready to move!
Case Studies: Successful Real-life Examples of Using AI-enabled Laboratory Billing Solutions

AI from theory is now moot; it is here to return real value to laboratory billing. Below are real examples of laboratories that reformed their billing through AI application.
Mid-size Diagnostic Lab: Fighting Claim Denials
Claim denials for a small diagnostic lab producing a lot of billing data were due to improper coding and lack of documentation to support the claims. Within three months after introducing the AI-enabled claims-scrubbing tool, claim denial rates were lower by 35% for the lab.
- Results: Claims were now approved quite fast with drastic reduction in the amount of multitudes of administrative work encountered previously.
- Added benefits: The AI system further gave feedback on the commonest errors met in giving directions for further process improvement for the team.
Regional Pathology Group: Speeding Up the Money
This regional pathology group is having concerns related to the delay in reimbursement. This is evident in the manual entry of billing data being delayed.
Here, they implemented an AI data-extraction tool interfaced to their EHR system. Now billing time is reduced by a whopping 40% due to automation, which makes for better claim submission speed.
Outcome: Payment cycles are now down to an average of 30 days instead of 60 days.
Also Benefit: Staff were now focusing their efforts on patient care instead of performing repetitive administrative tasks.
Large Lab Networks: Making Compliance Simple
Among the challenges faced by a large laboratory network composed of multiple locations is the ever-changing payer regulation, which has to be monitored for compliance. Thus, they implemented an artificial intelligence solution to monitor compliance in real time and flag possible risks in billing submissions.
Outcomes: Total abstention from compliance violations in the first year after implementation.
Added Benefit: Time spent on audit preparations reduced by 50%, keeping efforts of different degrees from being spent during reviews.
Independent Lab: Cash Flow Boosts
A private lab discovers unusual kinds of enzyme tests that produce inconsistent cash flow due to inconsistent timings of reimbursements. AI analytics forecasted the time trajectories for payment delays and the specific issues causing the delays.
- Outcomes: 25% improvement in cash flow consistency over six months.
- Other Pivotal Benefit: The lab used this information to negotiate better terms from the insurance.
Case in point epitomizes AI not just as a tool but rather a possible solution to continuous problems in lab billing. This would surely lead to optimize efficiency and better financial results as well as easier operations.
Please let me know if you are ready for the conclusion or should first discuss another aspect of AI in laboratory billing.
Conclusion
The laboratory billing processes have always remained tedious, complex, and error-prone, but now Artificial Intelligence promises to become a very strong solution. It has reduced manual intervention and errors and generated real-time analytics which can help the labs in addressing billing challenges, like claim denial, compliance issues, and inefficient workflows. Thereby reducing the time required to address some of those issues, it also creates faster payments and better cash flow with actionable insight.
With AI, Lab Managers, Healthcare Administrators, Hospital Management System providers, billing solution providers, and Pathology Managers can future-proof their operations rather than adopt an obligation to keep up with technology. There are fewer errors, faster reimbursements, and fewer bottlenecks in the billing workflow for all involved.
“The Task may appear rather formidable with immediate AI adoption, yet the words from live instances say otherwise. With evaluation of current equipment, the proper selection of tools, and team training, your lab could capitalize on accessing the advantages or benefits of AI without breaking the bank.”





