U.S. hospitals now rely on Electronic Health Records (EHRs) as one of their most transformative electronic healthcare systems. They are not just replacements for painful paper records; these systems are supposed to change how patient care works altogether, administrative efficiency, and medical data management. EHRs are now forming a pillar for hospitals to improve outcomes and increase operational efficiencies.
This post will assess how EHRs are being developed in the U.S. hospitals, what benefits they bring, and the challenges faced by health practitioners, administrators, and tech companies themselves. By the time you finish reading, you would have an image of the footprint of these systems in shaping modern healthcare and the road ahead.
Evolution of Electronic Health Record Systems in the U.S.

The electronic health record (EHR) in the United States has come about as a consequence of progress in technology and transformation through regulation. Paper-based systems once sufficed for constructing information on patients in hospitals, but the momentum for digitization started to creep in during the early 2000s. In reality, the HITECH Act of 2009 brought about the major impetus: it made finance available to healthcare organizations that adopted certified EHR Software using reimbursement based on its “meaningful use.”
Modernized care was not at stake but rather enhancing care by greater access, accuracy, and security in health information. Within the last decade, adoption soared. Almost all acute care hospitals use certified EHR systems in the United States today, creating a foundation for improved communication between health care providers and improved patient outcomes.
At the same time, this rapid replacement of paper systems had disadvantages. Paper-to-electronic transition needs large investments in training, finances, and planning: all these challenges highlight thoughtful implementation strategies, especially in resource-poor hospitals.
The Advantages of Electronic Medical Records
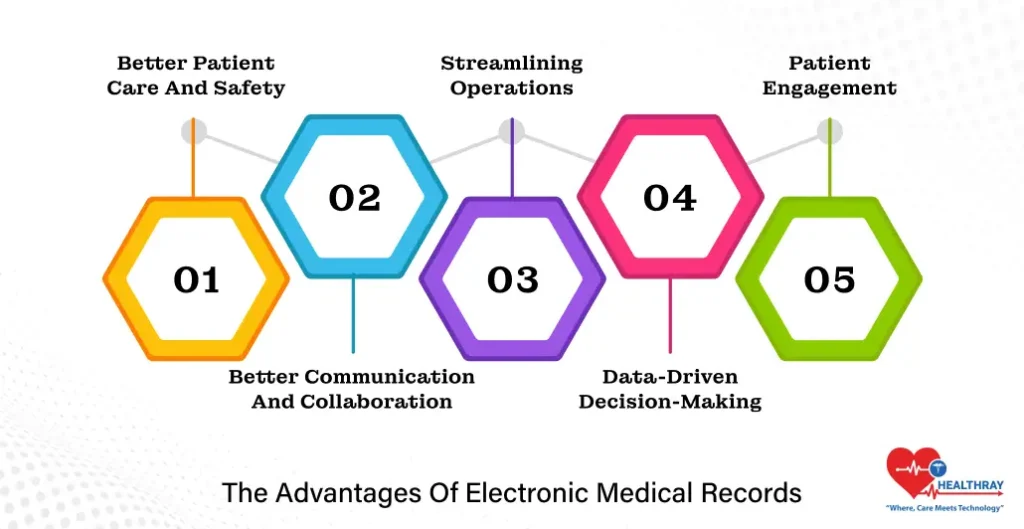
The advent of Electronic Health Records has ushered in an era of unexplored possibilities for healthcare. Far from convenience, they are quality enhancers, ensuring better communication and efficiencies that had been inconceivable with paper records. Here are some of the most important benefits:
Better Patient Care and Safety
An EHR gives a healthcare professional instant access to a patient’s entire medical history, lab results, imaging reports, and medication details. A comprehensive view can help prevent errors, such as a medication interaction, and ensure individualized care. For example, many systems have built-in alerts for allergies or critical conditions which protect patients against avoidable risks.
Better Communication and Collaboration
EHRs connect the siloed providers. Access and sharing of patient information of specialists, primary care doctors, and other clinicians have now become seamless. This reduces the redundancy of testing and ensures that everyone involved in the patient’s care is on the same page.
Streamlining Operations
Hospital administrators are recipient of the flow efficiency created by EHRs. Scheduling, billing, and compliance reporting are automated, saving time and reducing administrative burdens. Additionally, it provides better resource allocation, like real-time monitoring of bed availability.
Data-Driven Decision-Making
EHR – health records now become a goldmine of data available for physicians and health care managers. Simply analyzing the trends of patient outcomes or learning about the bottlenecks becomes easy. This data may even shape larger health interventions, such as public health initiatives or quality improvement programs.
Patient Engagement
Hauling the patient to the table would mean EHRs taking patients on an active engagement with patient portals. Patients test results, makes appointments, and communicates directly with providers in portals such as these. These facets of transparency build trust and improve relationships with providers and patients.
It is clear, however, that in order to realize their full potential, EHRs will need to be continually refined by ongoing collaboration between a range of healthcare professionals, administrators, and tech companies.
Challenges in Implementation and Use of EHR in Healthcare
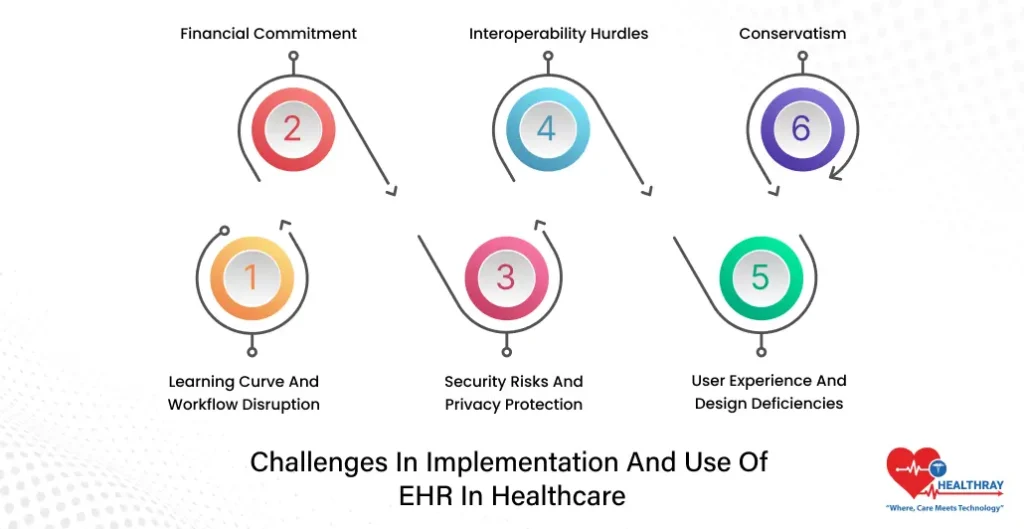
Electronic Health Records (EHRs) have transformed healthcare; however, their implementation and use have faced many challenges. These include the differences among healthcare providers who wish to optimize systems and their administrators, as well as tech companies.
Learning Curve and Workflow Disruption
In the hands of medical professionals, moving to EHRs often means changing and retraining on new workflows. The learning process can be lengthy and frustrating, especially when the systems disrupt existing rhythms of patient care. In busy hospital environments, each extra click or delay matters.
Financial Commitment
The expenditures accompanying EHR system setup must be handled by hospital administrators. Apart from initial purchasing, there are also overhead expenses such as maintenance, updates, and staff-training costs. These expenses could prove to be a deterrent for small hospitals with limited budgets.
Security Risks and Privacy Protection
EHR systems deal with highly sensitive patient data and thus offer a tempting target for hackers. Ransomware and data hacking incidents have revealed vulnerabilities, even in apparently secure systems. For countless healthcare organizations, safeguarding data against attacks and remaining compliant with standards like HIPAA remains a challenge.
Interoperability Hurdles
The promise of EHR systems was to improve sharing of information; however; many systems still remain unintelligent or not interoperable. Conflicts arise in hospitals using varying platforms when exchanging patient data, resulting in delay of care or partial clinical history.
User Experience and Design Deficiencies
Most EHR systems were constructed on the basis of maximum efficiency with little consideration for usability. EHR systems have received scathing critiques from health professionals for being overly complicated, requiring too many unproductive steps, or not matching real-world clinical workflow, adding frustration to overwhelming workload, frustration that occasionally manifests as outright burnout.
Conservatism
Change means culture; adoption of EHR may infuse a cultural change while not all will elect to participate. Some of the resistances may come from preferring the old, distrusting new technology, or foreseeing that their changing roles will be adverse.
Collaboration between healthcare organizations, managers, and the technology developers is required to meet these challenges. Solutions should give preference to a user-friendly design, comprehensive training, and seamless integration into clinical workflows.
Role of Technology Firms in Revolutionizing EHR Systems

EHRs have often presented challenges, which technology firms have managed to mitigate, rather than overcome. They have worked very hard to remain proactively at the fore of what in EHR innovation could be rethought, redesigned, or made better. So, utilizing all that they have to improve systems that already work well, they bring digital tools to bear on ideas that they would never have had without their expertise.
Simplification of User Interfaces
Rather than entering the textual readings, tech firms are working on systems that are so intuitive, they are almost fully user-dependent. The new architecture prioritizes efficient delivery of services, thereby drastically reducing the amount of time spent on administrative tasks; indeed, humanization toward a rebalanced care model is in line with advances in technology.
Improving Interoperability
This is the main thing to be achieved with regard to the bridging of data. Corporations are developing platforms to connect different EHR systems together. Commonization through standardized APIs and cloud applications allows a smoother exchange of data amongst hospitals, clinics, and other care providers, thus promoting far-reaching collaborations and minimizing treatment delays.
Use of AI
By implementing AI, EHRs are changing forever looking at automation through the lenses of data input loads, predictive analytics, policies, and clinical support. In practice, machine learning algorithms could be the ones pointing toward potential medication errors or patient chances or even proposing possible personalized treatment plans, based on historical data. This will take healthcare-related activities in the realm of high accuracy while reducing the cognitive workload on the real action takers within the profession.
Enhancing the Security of Data
The increase in cyberattacks, which target attacks against health care, pushes tech companies to put in place advanced measures of security such as blockchain, multi-factor authentication, and real-time monitoring systems. These technologies are meant to protect patient data along with a strict adherence to regulations.
Wearable and IoT-Driven Integrations
Currently, EHRs are embracing restrictions on data intake from wearables and IoT sensors attached. The system-embedded himself will react accordingly to changes in the patient-under-monitoring’s vital signs, hopefully providing a pre-emptive care before the catastrophe occurs and generally much better in chronic disease cure.
Small Hospital and Clinic Support
Fully aware of the financial constraints for the small-sized healthcare providers, tech companies have created solutions that are scalable and affordable. These EHR solutions that rely on subscription-based models, cloud hosting, and flexible pricing have successfully enabled the less resourced health institutions to adopt them for their clinical workflow.
Continuous Innovation via Collaboration
This innovative spark is collaboration between tech behemoths and healthcare organizations. The likes of Microsoft-Epic Systems or Google Health-hospital networks are rewriting the rules of what EHRs can do, from improved voice recognition documentation to smart patient data analytics.
Tech companies are more than just vendors but partners in Bray-changing health systems. They address the problems of current times and then innovate for problem resolution, thus forging the path into an even more unified and efficient health-care structure.
Conclusion
Health care in the United States has been preserved by Electronic Health Records (EHRs). From adding to patient safety to enhancing operations of hospitals in the country, the advantages of these systems are numerous. Nevertheless, the journey to EHRs might face challenges and hiccups even before being fully accessed. Whereas healthcare professionals want systems assisting in their workflows, administration should manage cost change, while the technology companies ought to come up with innovative ways for interconnecting and securing data.
The collaboration is the future for EHR. Nothing but a union of healthcare providers, administrators, and tech developers has the capacity for an unending prosperity in the existence of a seamless, efficient, and secure EHR. Such partnerships will address current ills that our hospitals are faced with and unlock possibilities in personalized medicine, artificial intelligence integration, and data-driven decision-making. Ultimately, Hospital Management Systems are not mere electronic records-an epitome of a modern healthcare framework building for better outcomes, operational efficiency, and patient involvement. EHR would need constant refinement just to keep simple things in a working order in any further progressive healthcare in the U.S.