Summary
RIS and EMR integration incorporates the imaging and clinical data in harmony. Further, when systems are connected, workflows become simple. Patients get reports quickly. Errors are fewer. Doctors can peer into patient history and imaging at a central place. It helps radiologists make timely and highly influential decisions. This ecosystem focuses more on practicality than technological progress. Medical supervision becomes facile. The collaboration becomes more lucrative. Healthcare workforce duties become incredibly lenient. Simply put, a connected system yields more favorable results!. I’ll go over how RIS and EMR integration can provide radiologists with unconventional ways to carry out daily operational tasks in this blog. Keep reading!!!!
Introduction
Clinics need to be accurate and on time in the fast-paced world of healthcare today. Nowadays, keeping Radiology Information System (RIS) or Electronic Medical Records (EMR) in different systems is an outdated approach. Integrating RIS with EMR makes the workflows clear and connected. First patient xrays reaches RIS and immediately scynchronise with EMR. This expedites decision-making, as doctors get the entire patient history in a single dashboard.
They don’t need to switch multiple systems to prepare a single report. Further, radiology workflow automation software integration with EMR minimizes the hustle and bustle of manual entries and delays. This integration is not just aimed at efficiency. It creates an ecosystem where data flows freely. Reports are accurate and communication is effortless among all the departments.
Radiologists and clinicians work in the same rhythm, making the patient experience smooth and trustworthy. When RIS and EMR merge together, they make the health service facilities more intelligent and agile. Technology streamlines, accelerates and ameliorates the dependability of the patient experience while operating silently in the background.
Understanding RIS and EMR Basics
RIS: Imaging Operational System
Radiology Information System (RIS) manages the practical work of radiology departments. Furthermore, features like scheduling, reporting, billing, and modality tracking are the core operations of RIS. RIS software makes the workflows feasible and transparent.
EMR: Patient Data Central Record
Electronic Medical Records (EMR) contain the exhaustive diagnostic documentation of patients. Furthermore, personal health history, lab analysis, diagnoses, and treatments are preserved in a single database. Thus, it provides longevity visibility to clinics.
RIS Responsibilities in Daily Imaging Operations
Radiology software supervises the imaging lifecycle. Furthermore, it can easily manage order creation and worklist management, report generation and turnaround tracking.
EMR’s Role in Longitudinal Patient Care
EMR provides an end-to-end clinical view to referring physicians. Furthermore, it ensures past encounters and imaging results are available in a consistent context.
Challenges of Disconnected Systems
When RIS and EMR are integrated, then manual data transfer becomes common. Furthermore, it creates duplicate entries, reporting delays, and data inconsistencies.
How Integration Aligns RIS and EMR
Radiology information systems integration synchronizes with patient demographics, imaging orders, and diagnostic results in real-time. Furthermore, both systems work in a single source of truth.
Building a Connected Imaging Ecosystem
RIS–EMR integration creates a connected foundation where workflows are efficient, errors are less and patient care becomes timely and reliable.
Advanced Integration Architectures
Microservices-Based Integration Design
Modern RIS–EMR ecosystems leverage microservices architecture. Furthermore, this makes the system modular and scalable. This approach goes far beyond traditional HL7 to support flexible connectivity.
Role of API Gateways
API gateways enable controlled communication between RIS and EMR. Further, this simplifies secure data exchange, version control, and traffic management.
Event-Driven Clinical Updates
When imaging results are generated in an event-driven architecture, EMR receives instant notifications. Furthermore, clinics get real-time alerts; this significantly reduces response time.
Containerized Deployment for High Availability
Containerized deployments can handle peak hospital loads. Furthermore, digital transformation in radiology maintains uptime even during busy imaging hours. Plus, it eliminates downtime completely.
Hybrid Cloud Integration Models
Hybrid cloud models on-premise RIS security with EMR cloud scalability. Furthermore, secure VPN tunnels and RIS synchronize data without compromising compliance.
Edge Computing at Imaging Modalities
Edge computing preprocesses data on imaging devices. Furthermore, emr reduces latency before EMR uploads. Also, it reduces network load.
Vendor-Agnostic Integration Platforms
Vendor-agnostic platforms such as Healthray deploy modular adapters. Also, the system enables plug-and-play integration with custom EMRs.
Role of AI in Unified RIS-EMR Workflows
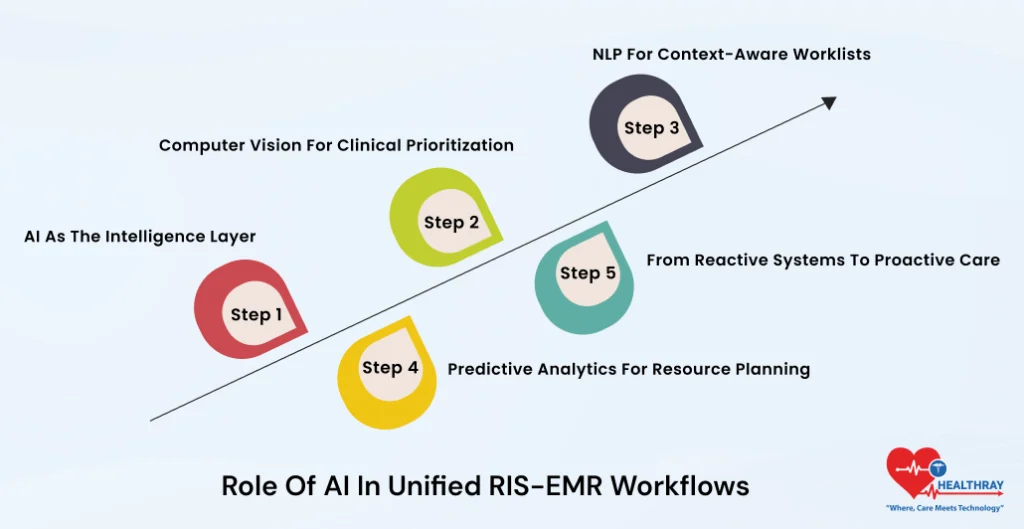
AI as the Intelligence Layer
In Unified RIS–EMR workflows, AI is not merely an automation tool; additionally, it becomes an intelligence layer as well. Furthermore, integrated systems analyze EMR priors and RIS images and autopilot the reports. Thus, it minimizes manual efforts to a significant extent.
Computer Vision for Clinical Prioritization
Computer vision algorithms detect anomalies in imaging studies. Furthermore, it automatically flags urgent cases and activates priority queuing in both the RIS and EMR.
NLP for Context-Aware Worklists
Natural Language Processing (NLP) extracts key critical findings from unstructured EMR notes. Furthermore, this information enriches RIS worklists. This helps radiologists read relevant context just before the scanning process.
Predictive Analytics for Resource Planning
AI-based predictive models forecast future trend volumes by analysing emr trends. Further, this makes the staffing, equipment usage, and scheduling more accurate and efficient.
From Reactive Systems to Proactive Care
This AI layer converts the ecosystem entirely and makes the practices more proactive. Furthermore, Triage automation reduces the radiologist’s stress decisively and helps radiology make expedient and sustainable decisions.
Optimizing Revenue Cycle Management
Unified Billing and Coding Intelligence
Integrated RIS–EMR systems use unified billing engines. Furthermore, it instantly reconciles RIS procedure codes with EMR diagnoses. The outcome greatly reduces the claim denials.
Automated Claim Scrubbing
Automated scrubbers validate CPT and ICD codes before claim submission. Furthermore, this process eliminates coding mismatches and avoidable rejections at the early stage.
Faster Remittance and Cash Flow
Electronic Remittance Advice (ERA) remittances directly flow into shared ledgers. Further, this expedites the reimbursement and improves overall cash flow significantly.
Denial Analytics for Root-Cause Resolution
Denial analytics dashboards highlight recurring patterns such as missing EMR priors and documentation gaps. Further, teams quickly identify root causes and can conveniently take corrective initiatives.
Adaptive Multi-Payer Rule Engines
Multi-payer rules engines dynamically adapt claims as per different payer requirements. In Connected setups ,clean claim reach is up to 98%.
Enhancing Patient Engagement Features
Patient Portals as Engagement Hubs
RIS–EMR fused patient portals provide MyChart-style access where patients can focus on images, reports, and exam preparation instructions. Furthermore, post-exam clarity makes the patient’s confidence strong.
QR-Based Personalized Journeys
QR codes during check-in connect patients with personalized digital journeys. Furthermore, this minimizes front-desk dependency and appointment no-shows.
Smart Scheduling with Patient Preferences
Automated reminders pull allergies and patient preferences from the EMR and align it meticulously with RIS scheduling. Furthermore, this makes the treatment plans customized based on the patient’s physical symptoms. Also, it is completely safe to use.
Continuous Feedback Through Surveys
Post-procedure surveys directly feed into unified analytics. Furthermore, hospitals can directly track patient satisfaction in real time and also quickly identify service gaps.
Telehealth-Enabled Imaging Follow-Ups
Telehealth bridge extends EMR video consults with RIS image sharing. Additionally, radiology data security software makes virtual follow-ups easier, saving patients from having to make additional appointments.
Step towards digital era with our healthcare solution
Revamp your hospital facilities and embrace change for better healthcare management. Ease in managing and organizing large medical datasets leads to effective analysis. Seize the opportunity now!
Multi-Site and Enterprise Scaling Strategies
Federated Architecture for Multi-Site Networks
Federated architectures synchronize RIS–EMR systems across satellite clinics and main hospitals. Furthermore, Central FHIR repositories make the shared data exchange structured and consistent.
Enterprise Master Patient Index
Master Patient Index resolves enterprise-wide duplicate records. Furthermore, this maintains a single trusted record of patients. It does not consider location; professionals can execute the treatment process from any location.
High-Availability Disaster Recovery Design
Active data centers and geo-redundant storage make the disaster recovery sturdy and powerful. Furthermore, through this setup, the system can exhibit 100% uptime. High uptime is extremely important for enterprise health care facilities.
Bandwidth Optimization for Imaging Access
Bandwidth optimization techniques compress image previews and enable emr embeds without requiring the transfer of complete DICOM. Furthermore, It minimises network load and provides fast speeds.
Scalability and Stress Testing
Scalability testing simulates 10x growth scenarios. Further, this ensures query performance or system response remains stable even during high loads.
Vendor Selection Criteria for Integration
Interoperability-First Vendor Evaluation
During vendor selection, it is highly crucial to select an RIS platform that delivers assembled FHIR accelerators and validated integration solutions. Furthermore, benchmarks like SLA clearly define the system reliability.
Roadmap Alignment and Future Readiness
Vendor product roadmap should be perfectly aligned with industry standards. Additionally, this guarantees that RIS-EMR integration is prepared for future technological or regulatory changes.
Proof of Concept Under Real Load
POC trials shouldn’t be restricted to demos. Also, measure sync latency under real-world workload to get a clear picture of actual performance.
Security and Compliance Validation
Insist on SOC2 Type II reports to verify vendors’ security controls. Furthermore, this helps radiologists objectively assess patient data protection and compliance posture.
Total Cost and ROI Assessment
Include hidden integration fee total cost models. Then, compare it to ROI projections over a three-year period. As smart selections ensure long-term financial discipline.
Long-Term Ecosystem Evolution
Governance for Continuous Alignment
In long-term RIS–EMR ecosystems, sustained governance continuously oversees committees’ standards adoption and vendor performance.
Continuous Audits and Optimization
Annual audits refine integration on the basis of emerging industry benchmarks. Furthermore, this approach no longer keeps the system in static mode; instead, it continuously improves it.
Data Lakes for Benchmarking Intelligence
The data lakes prepared from RIS–EMR fusion empower peer benchmarking. Furthermore, organizations can compare the performance and drive competitive advantage.
Conclusion
RIS–EMR integration transforms the isolated functions of the radiology department into a connected imaging ecosystem. Forward-thinking providers, especially those who use Healthray, lead this transformation and eliminate standardization waste and rework and are capable of plugging in AI, analytics, and future digital tools.