EHR has already become one of the very foundations of healthcare, with the aim of providing easier access, security, and order to patient information. Although the benefits of EHR systems are very clear, the road to successful implementation can be extremely convoluted. Healthcare providers struggle with various challenges, including ensuring data accuracy, managing internal team changes, and protecting patient privacy.
For healthcare leaders, technologists, and physicians, it is essential to grasp the “why” behind implementing EHRs. Successful EHR adoption is not simply a matter of complying and ticking boxes or moving away from paper records; it is about transforming the way healthcare is delivered to achieve better, faster, and informed care delivery to patients.
The steps leading to the successful implementation of an EHR Software will always include an assessment of readiness, training of personnel, and security of data. This guide will go through these best practices, focusing on a smooth, practical approach for EHR solution implementation that can satisfy the needs of healthcare as well as patients.
The following sections will detail duty-imposing implementation steps for successful EHR integration, strategies to circumvent common pitfalls, and approaches to maximizing the potential of EHR systems toward improving patient experience and efficiency in delivering healthcare.
Key Steps for Best EHR Practices
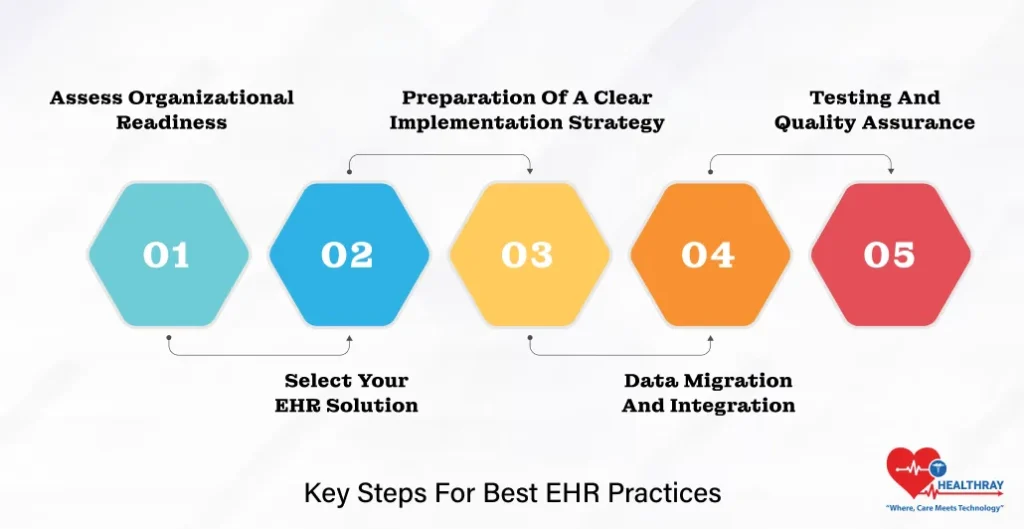
Taken stepwise, launching an EHR (Electronic Health Record) system successfully may improve implementation with impeded workability, increase user frustration and even jeopardize patient care. The following are some very basic steps necessary toward an efficient rollout:
Assess Organizational Readiness
No two healthcare organizations are ever the same; they have different needs, resources, and challenges. Therefore, appraise what is working, what is not working in terms of workflows, what is available for technological infrastructure, and what is ready at a human resource level to evolve. Involve key participants at the beginning: clinical staff, administrative staff, and IT personnel. Knowing where the gaps are directs the subsequent decisions on the right EHR system to choose and how to prepare your staff for the ensuing changes.
Select Your EHR Solution
As discussed before, EHR solutions are not universally applicable. Systems that are congenial to the size and specialty of the organization and meet integration requirements should be considered. User-friendly interfaces, applicable safety standards, and compatibility with existing technology should be sought. Priority should be given to usability: interoperability is also very important, so the staff may concentrate on patient care, and not wasting time trying to negotiate a cumbersome EHR application.
Preparation of a Clear Implementation Strategy
A structured implementation plan keeps everyone on course. This preparation should involve phases, timelines, budget expectations, and specific goals. Many organizations feel that a phased approach, starting off from the pilot program within one department, would help identify potential points of resistance before they affect the organization in large. This lends time for other departments to fine-tune their processes and provide feedback before full-blown implementation.
Data Migration and Integration
Data migrations out of legacy systems or the paper world must be carefully engineered. Commence with analyzing which data would have the high priority for migration and put in place procedures to check the accuracy of those data. Coordinate with the technical staff and integration teams to achieve seamless integration with downstream processes like billing, lab results, and imaging. Well-executed data-migration processes would mitigate disruptions and preserve patient care continuity.
Testing and Quality Assurance
Testing is a continuous process stretching across the implementation phases. Execute simulated scenarios and allow staff to perform their daily tasks on the new system to effectively assess risk. Testing secures a path for the intended function of an EHR system when it goes live to back the team without major disruption. Through these core steps, EHR lays the foundation to turn healthcare providers into successful players. Engaging teams from day one, using the right tools, and testing thoroughly limit the costs of set backs and guarantee a system that works to the advantage of patient care and efficacious workflows.
Information on Training and Support Best Practices

Perhaps the most important aspect of an EHR implementation is that all team members should know how to use the system. It matters little how sophisticated the technology is; its worth depends on the confidence and competence of people using it. A comprehensive supportive training approach will help reduce resistance and enhance the adoption of the system; most importantly, the staff will be able to appreciate the tangible advantages of EHR in their daily work.
Provide Role-Based Training
Not all users interact with an EHR the same way. Rather, doctors, nurses, administrative staff, and IT professionals all have their own needs and responsibilities within the system. A training program targeted toward these functions ensures that the appropriate subjects are taught, making for a much more effective and efficient learning process. Focused education minimizes wasted time and prepares each individual to use the EHR feeling confident by the end of it.
Hands-On Training and Simulations
Real-time, hands-on training provides users with wise practice in a controlled environment. Simulations should be set up for situations typically encountered in daily practice. Such activities help to reinforce system functions, enabling team members to practice actual data entry, patient information retrieval, and troubleshooting without felt pressure. Familiarization through practice in a safe environment plays a big role in error mitigation when the system is allowed to go live. To further strengthen learning outcomes, mentor mentee matching supports personalized guidance during training, allowing experienced users to help others build confidence and master the system more effectively.
Constantly Offered Support and Resources
EHR training should continue beyond the initial training. Regular follow-up sessions and workshops, as well as accessible resources quick reference guides or video tutorials will help keep knowledge fresh and available for staff questions as they arise. Ongoing support helps team members feel confident and engaged with the system. Be sure to have an assigned EHR support team to tackle problems as they arise.
More Feedback Shows A Lot
Feedback from staff who use the EHR daily is extremely valuable. Encourage open communication regarding the positives and pain points they have encountered with the system. Having that feedback loop enables the organization to improve the user experience while demonstrating to staff that their input is of value.
Keep a Party on All Milestones and Recognize Developments
The journey from one EHR to another can be a painful affair; thus, recognition of the immense work of the staff goes a long way. Celebrate the milestones of project implementation such as completing training or a score against a set target. Recognition of individuals and groups will help in creating a happy atmosphere around the EHR system and enhance morale.
A comprehensive approach to training and support ensures that healthcare groups have an adequately trained and confident team that can maximize EHR technology. Supported staff members act in a much-smoother operation and patient interactions, endorsing an overall positive shift towards healthcare services.
Improving Patient Satisfaction and Data Protection

The perfect story of a Best Electronic Health Record System really comes true when it helps the health service provider to satisfy the patient experience in turn. Patients benefit from these EHR from directly getting access to their health information, communicating with providers, and improving transparency. Data security also becomes imperative in these types of scenarios to safeguard the interests of a patient regarding privacy as well as the different regulatory standards.
Empower Patients with Access to Their Health Records
One of the standout benefits of an EHR system is granting patients the ability to access their medical records. The patient portals allow patients to review their test results, track their health over time, and even update personal information, ultimately reducing the administrative load on the healthcare provider. By putting the control of their health information in the hands of the patients, the EHR empowers patients to make informed decisions and meaningfully participate in their healthcare journey.
Facilitate Better Communication Between Patients and Providers
Integrated into the EHR system is a system for patients to communicate with their healthcare providers. Patients can follow up with clinical questions, receive instructions for care, and clarify their treatment plans through EHR messages without the need for an in-person visit. These buildups in communication also instill trust and assurance in their patients across appointments.
Ensure Robust Data Privacy Measures
Patient data security is crucial. An EHR system implementation must entail the protection of sensitive health information against unauthorized access, accidental disclosure, and loss. Strong data protection requires state-of-the-art encryption protocols, multi-factor authentication, and strict access controls. Regular security audits and compliance checks help to maintain continual adherence to privacy standards, such as HIPAA and any other relevant regulations.
Educate Patients About Data Security
Patients may have a genuine concern for how digitalization is going to affect their stored health data. When potential patients are given proper and easy-to-understand information regarding all measures taken to protect all their data, it breaks away most, if not all, of the concerns. By informing the patients about encryption and privacy practices and security, it provides a level of comfort to them that all their data is secure. The more-informed patient is more likely to accept and trust the system.
Streamline Administrative Tasks for Faster Patient Service
EHRs contribute to alleviating administrative burdens and automating basic activities that take away actual patients’ time from health care delivery. For example, EHRs automate appointment reminders, simplify billing processes, and store insurance information; hence, these features help expedite service delivery. Such observable features are, therefore, highly appreciated by patients, thus contributing greatly to a better healthcare experience.
Evaluating EHR Success and Future Trends
Once the EHR system is up and running, it must be measured for efficacy and impact. EHR system success evaluations assist in ensuring that the organizational goals are met by EHR systems in enhancing patient care and utilizing caregivers effectively. Future considerations in the evaluation allow the caregivers to be prepared for the next generation in EHR technology for easier adaptation and evolution in their operation in light of new inventions.
Define Key Performance Indicators (KPIs) for EHR Success
It is very important to track the metrics accordingly to assess how well their EHR system really supports healthcare operations. Common KPIs include patient satisfaction score results, hours spent in documentation, the error rate in patient data, and total system downtime. Healthcare organizations can, therefore, establish and track KPIs in order to identify areas of improvement and confirm the benefits of their investment in EHRs.
Monitor Staff Adoption and Satisfaction
Staff adoption and usage of an EHR system in their day-to-day lives typically dictate the system’s usefulness. Get in touch on a regular basis with team members to keep track of their experiences and to ask for input regarding any problems they face. Satisfaction among healthcare providers implies that the system is intuitive, well integrated into the work processes, and in line with what they need.
Assess Patients Outcome and Efficiency in Care Efficiency
One of the primaries objectives of EHR is to attain good patient outcomes in terms of accurate and appropriate health information. A review of patient outcomes, including effectiveness in treatment as well as re-admission rates, determine whether or not the EHR system has improved the quality of patient care. Monitoring also includes the efficiency of care in terms of shorter waiting time and smoother processes resulting from the EHR application in an organization.
Keep Abreast of New Developments in EHR Tech
New technologies are mushrooming in EHR therefore, advances can be seen almost daily and new features and functions are continuously being integrated. Artificial Intelligence applications in predictive analytics, development of telehealth, and personalized medicine feature in the major trends. These trends will guide health organizations in preparing for an upgrade in the use of their EHR systems in the near future.
Plan for Continuous Improvement
EHR adoption is not a one-off endeavor. Updating the system regularly, conducting a refresher course for users, and auditing the processes ensure that the EHR system changes over time to capture changing health needs. Hence, establish a plan for continuous improvement that will include routine audits, user feedback sessions, and periodic retraining for staff members. This guarantees that the EHR would remain a dynamic and flexible tool with regard to optimizing patient care.
No healthcare provider will ever go wrong by evaluating EHR success trends and then constantly improving upon it. Continuous improvement keeps an EHR resource dependable, up-to-date, and ready for anything the future brings in modern healthcare.
Conclusion
Successful Installation of Electronic Health Records System: Appropriate electronic health record installations significantly impact healthcare institutions because, despite the effort, benefits will outweigh costs. An effective EHR system streamlines the flow of activities, enhances patient care, and ensures data availability as well as the security of healthcare organizations. However, achieving these results requires good planning, training, and follow-through for continuous improvement.
Preparing and planning Early preparation and planning form a solid foundation for successful implementation of a Hospital Management System. Bringing on-board all stakeholders from the very beginning, therefore clarifying the objectives, helps to minimize disruptions associated with the implementation process and also suggest how the EHR will fit into the organization. Customized training is also an important factor to achieving users’ buy-in as the training based on roles ensure that all staff are confident in using the system. Teams are then able to keep improving skills and deal with issues as they emerge through continued support and feedback.
Accessing better and more secure patient data is perhaps the most important advantage of employing EHR systems. It allows patients to gain easy access to their medical records and therefore smoothens communication with the health providers; in turn, strict security measures ensure protection of patient details from outside access as well as compliance with various privacy regulations.
By measuring success and keeping an eye on future trends, healthcare providers can optimize their EHR investments. By measuring key performance indicators and evaluating how the system impacts on patient outcomes and staff efficiency, organizations are in the position to derive maximum value. In addition, health pros are in for continuous evolution as all new advancements and trends in EHR comes along.
However, adoption of an EHR requires regular, continuous updates, retraining, and performance reassessment to adapt to the changes in healthcare needs. Indeed, a well-designed EHR application stands ready not just to meet present needs but has a resilient, patient-centered digital health management that will assure continued effectiveness beyond today.





