Pharmacy and its software are reinventing the pharmaceutical environment from task automation to patient centric care. Improving, for example, medication optimization, patient-communication, etc., these systems are emerging as of outstanding value to deliver a clinically and patient-tailored experience.
So, how exactly do these solutions impact patient care? At first they facilitate the automation of more complex workflows making it possible for pharmacists to spend more time with patients as opposed to time spent on administrative chores. Software applications are used to reduce errors, increase medication adherence by patients, and increase access to care (e.g., telepharmacy). In this article, we’ll explore the different types of pharmacy software, key benefits to patient outcomes, and considerations for pharmacy owners aiming to implement these technologies.
Why Pharmacy Software is Transforming Patient Care?

Pharmacy Management System (PMS) is the new generation game changer for a day-to-day pharmacy. As effectiveness and patient centred care are increasingly demanded the role of pharmacies is evolving step by step and being filled with digital solutions, which aim at more convenient pharmacy operations,but most importantly to enhance patient care and patient satisfaction. Such types of software applications afford pharmacy operations the tools with which to be efficient in some of the vital functions, for example the management of stock, management of and retrospective analysis of patient information records, and dispensing of prescription drugs. All things considered the pharmacists will be able to shift their attention to quality patient care and not to administrative busy work.
Meeting Patient Expectations
Today’s patients anticipate prompt, easy services from pharmacies. Through the incorporation of functions such as prescription refills over the internet, patient reminders, and rapid information on patient medical records, prescription software has potential to meet these expectations. Along with patient experience, this access contributes to the compliance of prescribed drug therapies.
Minimizing Errors and Increasing Safety
Errors within pharmacy environments incur significant consequences because of carefully annotated patient histories and polypharmacy drugs. Through the detection of potentially inappropriate drug doses, drug or dosage interactions, software solutions incorporating features such as, clinical decision support systems (CDSS) can be used to reduce common errors. This through automation, human‑error is minimised and it is in the end the patient’s health who is saved.
Supporting Remote Care through Telepharmacy
Now that telepharmacy offers a means to bring care to remote or underserved populations, telepharmacy is an increasingly effective means with which to bring patient care to such populations. The telepharmacy service can be used to establish a dialogue with pharmacists over a webcam call, or chat, to be given drugs related guidance, and even to have electronic prescriptions. This technology enabled the spread of pharmacy care and spread of pharmacy care even to those living in regions with limited access to care due to the length of travel to care.
The fact that the object is capable of repositioning the pharmacy towards software-driven business models is also to keep up with competition, i.e., to have technology to make on time in order to outmaneuver the competition. Specifically, these digital tools can be used by the independent pharmacies to provide high quality care, without developing distance with patients.
The importance of software in pharmacy for patient care

Pharmacy software applications are available in a vast number, each tailored to a particular problem of pharmacy operation or patient interaction. Next, let us discuss the key types of pharmacy software and the corresponding direct impact on patient care.
Pharmacy Management Systems (PMS)
Purpose: Pharmacy Management System simplify everyday business, everything from inventory to billing to patient records.
Impact on Patient Care: These systems by automating routine procedures have an effect that they can release pharmacists time for patient interaction. For example, inventory management and automatic refilling provide sufficient medication, and throughput delays are kept to a minimum. E-prescribing integrations, however, not only eliminate the potential for errors to occur in prescription execution, but also deliver the right medication in due time.
Electronic Health Records (EHR) Integration
Purpose: Integration of the system into the EHR offers the pharmacist full and direct and continuous access to all information in a patient’s medical history and, as a consequence, the pharmacist is in a better position to perform a more individualized and specialist pharmaceutical care.
Impact on Patient Care: Pharmacists have access to www.ncbi.nlm.nih.gov, which allows them to observe, live, at all times what the patient has being taken by the patient, what the patient has allergies to as well as what the patient has been medicalized for in the past. This holistic view aids in identifying potential drug interactions or contraindications, enhancing medication safety. The deployment to EHR also facilitates better coordination among medical staff, pharmacists, to name some, for better care continuity, etc.
Telepharmacy Solutions
Purpose: Telepharmacy platforms enable pharmacists to perform virtual interactions and can provide patients living in remote or underserved regions with health care professional advice.
Impact on Patient Care: Telepharmacy enabling pharmacy patients access to, for instance, medication counseling or prescription refills without being physically present in the pharmacy. For individuals who do not have the ability to move, or for those who live in a rural area, this access to care ensures that they are able to continue receiving timely and uninterrupted care.
Clinical Decision Support Systems (CDSS)
Purpose: CDSS is based on data and algorithms to guide clinical decisions for appropriate patient care by pharmacists.
Impact on Patient Care: Based on patient data and comparison with clinical recommendations, CDSS can provide the pharmacists alerts about potential issues, such as drug interactions or incorrect dose. Through the use of this assistance, risks are minimized to the point that patients are given safer, better, care.
Patient Engagement Tools
Purpose: Patient engagement technologies (eg, mobile applications, automated communication platforms) assist patients in medication management and information acquisition.
Impact on Patient Care: These devices assist pharmacists in the provision of refill reminders, dosing suggestions, and education on medication use all of which contribute to excellent adherence. Patients also tend to accept a given medication treatment the first go around faithfully, in the right way, to be able to make health better.
These technologies are certainly useful to increase patient satisfaction, improving the safety of medicine and the quality of pharmacists care in pharmacies. Further, it is clear to pharmacy owners or operators that these technologies may be effectively and accurately used to support efficient and effective operations that can best meet today’s healthcare consumers’ needs.
Benefits of Pharmacy Software Solutions on Patient Outcomes
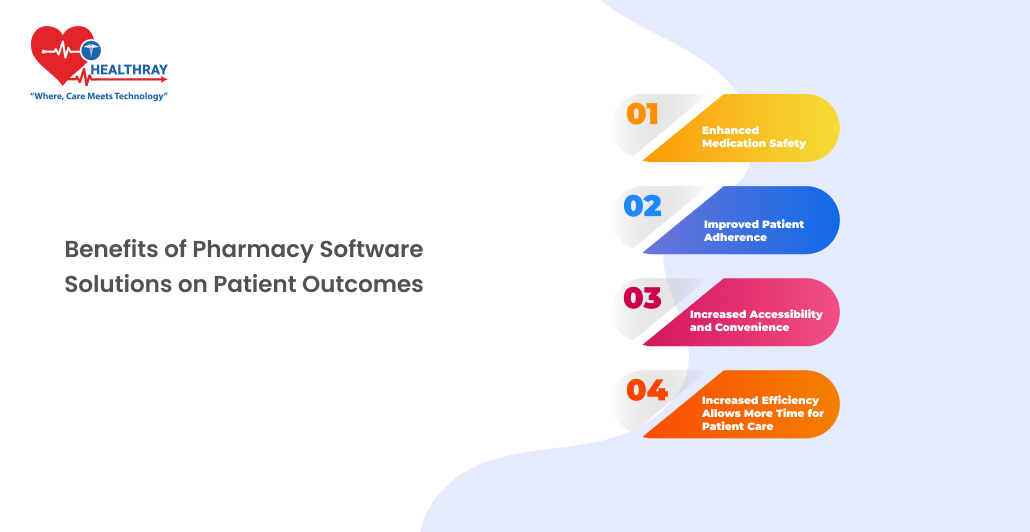
Pharmacy computer solutions, in turn, have direct implications for patient wellbeing/attrition, as well as medication safety, quality of life, medication adherence and pharmacy use. Following are some of the most effective ways in which pharmacy software solutions enhances clinical outcomes.
Enhanced Medication Safety
Error Reduction: Automating such systems (e.g., pharmacy management, clinical decision support) can decrease the incidence of human error. They alert the pharmacist to the risk of drug interactions, drug overlap, and wrong dose that significantly decreases the error rate of drug therapy.
Improved Accuracy: E-prescribing Devices provides ease of pronunciation, clear and unambiguous and uniflexible, which are similar to none other eliminate the errors that are often found in an electronic prescription. This also enables the pharmacist to confirm prescriptions more correctly and in turn, it helps us to avoid the wrong dispensing of the drug to a patient.
Improved Patient Adherence
Automated Reminders and Refills: The development of instrumentation that can be used to activate patients has emerged, for example, in the form of smart phone applications (apps) and SMS (short message services) reminders that can help to enforce adherence to prescribed drugs at the right times. Careful reminders refilled in a way that patients do not forget a dose due to expired prescriptions can lead to an increase in health outcomes, especially for patients with chronic diseases.
Education and Counseling: It is also possible to use software tools that allow for, e.g., immunizing against medical information (i.e., the adverse effects of drugs and correct taking of drugs), to pharmacists, for the patients. The more knowledge the patients have of the treatments they are pursuing, the better prospects they have of treatment adherence.
Increased Accessibility and Convenience
Telepharmacy Services: Telepharmacy enables patients in rural and marginal areas to receive expert advice and medication managing services without leaving the rural or marginal area directly to the pharmacy. Thus, by that portability, pharmacy services can reach those who cannot access a pharmacy or reside in a rural setting.
Multi-Channel Communication: Pharmacies can communicate with patients through multiple channels including mobile apps, online portals and automated telecallings, etc. Not only does this accessibility enable direct communication, but it also provides patients in an effective way with an opportunity to ask a question or, perhaps even, voice a concern, and subsequently promotes a more active outlook among patients in terms of their healthcare.
Increased Efficiency Allows More Time for Patient Care
Streamlined Operations: Automation of pharmacy inventory management and billing and record-keeping tasks lessens the pharmacist’s workload. This enables pharmacists to do more “patient contact time” rather than back-end work, which in turn means more time is available for patients-focused, high-quality, individualized care.
Data-Driven Insights: There are many pharmacy software packages with data analytic features that can equip pharmacies with the tools to analyze patients’ behavior, for instance, missed refills on a routine basis, such. With this, pharmacies have the potential to intervene in the early phase by providing reminders and counselling that will contribute to a better health outcome.
Through the utilization of these software programs pharmacies can build a safer and more pleasant environment for patients, which consequently leads to better care experiences and outcomes. This digitalization is proving to be critical for pharmacies to be competitive and meet patients’ needs in a continuously changing healthcare environment.
Case Studies of Successful Implementations
Use cases of pharmacy software installation demonstrate how these applications contribute to both the enhancement of patient care and to the optimization and increased efficiency of the pharmacy workflow. These are some case studies that demonstrate the tangible outcome of a digital solution(s).
Independent Pharmacy with Integrated Pharmacy Management System
Case: An independent pharmacy developed a comprehensive Pharmacy Software with electronic prescription functionality and automated inventory control. This could also be applied in a larger scope to interpret a larger number of prescriptions on a more detailed level without additional new staff, i.e.
Outcome: The system helped to increase medication correctness by minimizing inaccuracies in the dispensing. Patients got the medications quicker with less out-of-stock medication which improved patient satisfaction and patient loyalty. Automatic refill reminders of the system also generated a 20% reduction in patients’ non-compliance but also a positive impact for chronic medications.
Multi-Location Pharmacy Chain Using Electronic Health Records (EHR) Integration
Case: A network of community pharmacies integrated their software with Electronic Health Records (EHR) and pharmacists could access longitudinal patient outcomes in real-time.
Outcome: Pharmacists’ access to patient history, current medication and medication history—as well as allergy history—because of EHR integration allowed for prevention of medication interactions. In addition, pharmacists and physicians could work together to deliver personalized guidance to patients. This integration also contributed to a 15% decrease in adverse drug reaction and improved patient outcomes, especially in multiprescription patients.
Telepharmacy Expansion in Rural Areas
Case: To deliver pharmaceutical care to patients in geographically isolated rural populations, a community pharmacy implemented a telepharmacy service that provided both video consultations and prescription by electronic means.
Outcome: Telepharmacy provided essential services to rural patients who otherwise had limited access to pharmacy care. Patients could potentially have onsite consultations at their convenience and medication drug use counseling without the need to travel. This expansion contributed to medication adherence and satisfaction rates both increasing, and patients apparently found the ease and continuing care to be desirable under the curriculums geographic limitations.
Patient Engagement Software in a High-Volume Pharmacy
Case: A pharmacy with high demand employed a patient engagement platform with mobile-app based features, prescription tracking, dosing alerts, and pharmacist-to-patient direct communication.
Outcome: This platform led to improved patient adherence and fewer missed doses, particularly among elderly patients managing chronic conditions. Patients, by gaining instant access to their drug information, and the ability to text message back to the pharmacy, reported increased involvement in their health care and therefore, improved overall health status.
Conclusion
Streamlined operations, better patient outcomes, and stronger competitive standing. As digital tools are further built and utilized, pharmacies and pharmacy owners that utilize the tools will be best positioned to fulfill the dynamic needs of the contemporary health care. Systemic use of digital tools within hospital management system, telepharmacy, AI analytics and wearables enables pharmacies to provide faster, safer and more patient-centric care. Investing in such solutions could sound like a step too far at first, but the resulting benefit in terms of patient satisfaction, and patient loyalty, will likely outweigh the cost and be a success in the long run.
Implementation of these systems is also needed in order to ensure a future in which care is effective, affordable, and tailored on an individual basis, not just to follow the curve. Pharmacy software solutions create a bright future for pharmacies that can better respond to patients’ needs and improve community health outcomes, starting with pharmacies.