Electronic Medical Records (EMR) systems have changed the spectrum of care for patients’ records and form the basis of health care systems. EMRs take the place of conventional paper records by centralizing patient data digitally, enabling healthcare professionals to make better decisions more quickly. Yet, given all the options and technological jargon around, it is highly likely to be confused about how EMR software functions, what it is designed to achieve, and why it even counts.
The principles of EMR systems are discussed within this guide, as are the benefits EMRs offer to both small and large practices, and how to choose a suitable one. We’ll explain what matters in EMR software and why it’s something to consider for modern health care environments, whatever your goals may be—improve patient outcomes, accelerate administrative work, or ensure data security.
What is EMR Software?
Electronic medical records (EMR software) is a computerized health care delivery system where the patient’s health data can be stored and maintained. As a digital incarnation of the paper analogue chart. But digital storage is only one aspect of it. EMR systems provide physicians with a holistic view of their patient’s medical records in a single glance through structuring and presenting patient records, treatment, diagnosis, prescriptions and even laboratory values.
The main function of an EMR is to bring this information together to facilitate clinical workflow and thereby optimize patient care. Electronic medical records are often more tightly customized to individual practices, collecting and structuring patient data from the first visit onwards, compared with relation to EHR (Electronic Health Record) systems, which focus on data exchange between multiple practices. This emphasis guarantees that providers have access to current and accurate patient data, streamlines their procedures, and lowers errors.
Key Features of EMR Systems
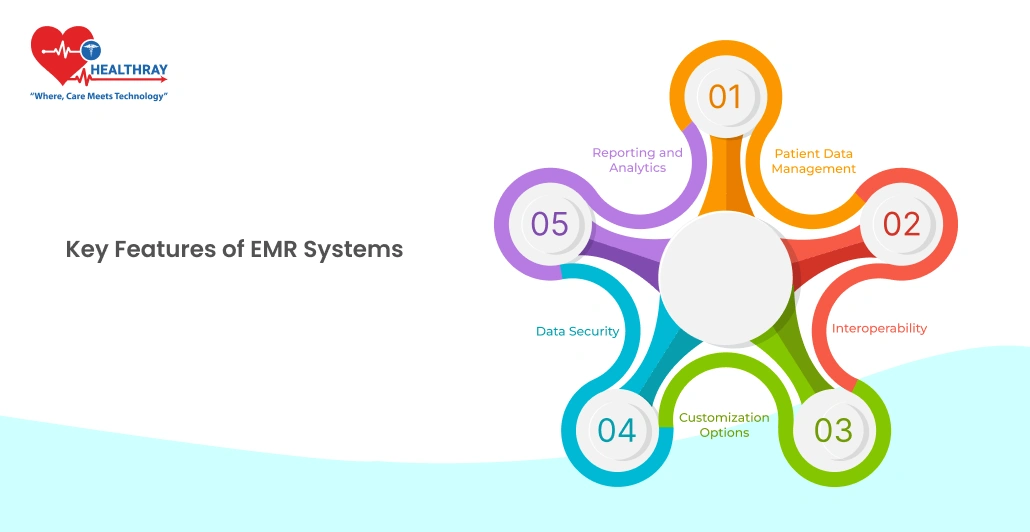
Understanding the inherent properties of an EMR system may be critical to maximize the function of an EMR system in health care facilities. The following are the main functions that constitute EMR software as a sophisticated instrument of modern medicine.
Patient Data Management
EMRs make, structure, and maintain a huge amount of patient information. From medical history and lab results to allergy information and current medications, the system keeps everything in one accessible place. This one storage enables providers to rapidly and effectively enter patient information, and can provide continuity and accuracy in care providing.
Interoperability
Interoperability is one of the most sought after functionalities in that it enables the EMRs to “speak” to other information systems, for example, imaging platforms or laboratory softwares. The data-sharing feature of this utility is very useful for offices that coordinate care between, or providers to, other providers or to a large number of services. Interoperability allows a more integrative approach in the management of patients, minimizes unnecessary testing, and accelerates referrals.
Customization Options
EMR software is also commonly employed to represent the fact that no two healthcare settings are the same by providing the opportunity for customization. Providers are able to change layouts, workflows, and templates, to the extent required by practice requirements. For example, a cardiology clinic would give more importance to the diagnostic and imaging details, and a pediatric practice to the fact of vaccinations. Practices can operate more effectively with these personalized options.
Data Security
Patient data confidentiality is always the top concern in every healthcare setting and EMR systems pay attention to security features, including data encryption and role-based access control. Encrypted EMRs contribute an additional security level to patient records by restricting data access to clinician job roles. In addition, many systems work according to medical regulation (e.g., HIPAA in the US) to ensure anonymity of individual data.
Reporting and Analytics
The growing functionality of community-based EMRs includes reporting and analytics features that allow to report some capabilities, follow the patient progression, identify the best areas to improve quality of care. Using data insights, health care professionals can, not only provide, accurate decisions in terms of patient care, operational efficiency, and even financial returns.
The following characteristics of EMR software allow healthcare practices to equally deliver quality, safe and patient-centered care, and therefore makes it an essential tool in the contemporary healthcare landscape.
Choosing the right EMR system for your practice.
Choosing an EMR system is a pivotal one, because once good decision, it can enhance both patient care, operational efficiency, and future development. Such as an algorithm for EMR selection to best meet the practice need.
Assess Practice Needs
Start by evaluating your practice’s unique requirements. Give weight to both practice scale, the nature of the patients you serve, and/or specific department examples of work flows. Instance, a pediatric clinic requires an EMR to keep track of the immunization history, whereas a practice in mental health will require the functionality for keeping track of therapy note. Clarifying your specific needs helps narrow down the features you’ll require.
Define Key Objectives
Clearly define your goals before deploying an EMR system. These aims may, e.g., consist of better patient care, better administrative effectiveness, better regulatory compliance or better error reduction, etc. By clearly stating the desired outcome, it helps ensure that the final decision is in line with the practice’s ethos and principles and also serves to benchmark against alternative systems.
Budget Considerations
It is important to establish your budget at an early stage, taking both initial costs (software license, installation, data migration) and ongoing costs (subscription, support fees, updates) into account. Consider the financial promises of each of these systems, and cloud-based vs. on-site systems. Low-resource practices may be attracted to cloud-based EMR billing system as they have a lower upfront cost, but must also take recurring subscription costs into account.
Evaluate Usability and User Experience
Usability of an EMR system is of great significance for a successful implementation. Select a system with a natural input interface, its easy navigation, and relatively few steps. A simple EMR [Can] significantly reduce training time and the level of employee satisfaction, as the employees perform the tasks in an effective manner. Wherever possible, demonstrations, or trial runs with next generation systems are recommended to evaluate the end user interface in situ.
Consider Interoperability
Clarify if other applications which you run, such as imaging, laboratory, and billing software, can be integrated into the EMR system. Coordinated care requires the seamless transfer of data among systems, and this is particularly important when your practice is sending or receiving data from others. In order to avoid data silos, make sure the system is compliant with interoperability standards of medical fields.
Prioritize Data Security and Compliance
Due to the nature of EMRs as containing sensitive patient data, seek out systems with strong security measures in place. Describe features including, data encryption, role-based access control, audit logs, and HIPAA (or corresponding standards around the world). Security-focused EMRs decrease the risk of data spills and Companies can not just stay compliant with the relevant regulations, but also preserve the trust of patients and the ability to operate a practice.
Assess Vendor Reputation and Support
Perform a study of EMR vendors’ standing, focusing specifically on customer feedback, number of years in business, and support offered. Good customer support can have a dramatic effect during the transition and ongoing maintenance. Select a vendor that has a history of successful implementations, a strong support system, and consistent updates to the software to keep your system operational and up to date.
Scalability and Future Growth
[Ensure] the EMR system is flexible enough to handle the scale of your practice. For example, assuming you intend to expand the scope of services or to serve more patients, a scalable EMR has the capacity to scale out to accommodate such expansion without having to reset the process. Scalability enables expansion to new users, features and integrations, and thus is an important factor in future sustainability.
If carried out in this manner, practices can choose an EMR system that not only includes vendors’ current features, but future vision as well, leading to a more efficient and less jarring transition.
Steps to Transition to an EMR System

Successful implementation of an AI-powered EMR Software System requires, however, a thoughtful plan to minimize interruptions and increase its uptake rates. Here are the essential steps for a smooth transition:
Plan the Transition in Phases
Adopting an EMR system is ideally undertaken in stages. Begin by outlining the transition schedule, defining important milestones, and identifying who will be responsible for each task to the appropriate team members. By breaking the process, it is possible to control every step, which in turn can mitigate disruption to normal operations. Consider whether the transition will be “easy” or whether there is a “go-live” date for the entire system (as one implementation will affect the workflow in a different way than the other).
Prepare for Data Migration
Data migration is the task of transferring existing patient records to the EMR system. This process may be tedious, especially when digitising paper documents. In view of optimal data migration, initially concentrate on the recently updated and generally accessed data. There will be some practices which will retain the paper versions of the older records for a limited time. To avoid data loss and still accurately model the process, it is crucial to have close collaboration with the EMR vendor modeling this process.
Train Your Staff Thoroughly
Training is an essential component for staff to feel competent and confident about operating the new system. Conduct training sessions that will be comprehensive, covering all facets of EMR software in many granular details, from data entry on patient administration to clinical workflow management. Interactive training (i.e., tactile skill practice, and mentor-assisted simulation) in general is judged to be most effective. Be prepared to give refresher education when needed, as both active learning and continuing education can both lead to improvement in the reduction of errors and the development of expertise with practice.
Customize the EMR to Fit Workflow Needs
The EMR system can be tailored to fit the work style of your practice and is anticipated to result in improved productivity and user satisfaction. Adapt the layout to meet those daily procedures, change templates, and develop forms specific to a particular specialty with the EMR provider partner. As this adaptation process is taking the system toward more routine behaviour, it reduces the number of learnings that the staff has to perform.
Test and Monitor the System
To successfully roll out the EMR system, put it through tests under controlled conditions. In doing so early problems can be detected and remedied before final release. Critical staff served as part of this test phase and provided feedback on ease of use of the system, system reaction characteristics and system effectiveness. L monitor the system after go-live and maintain its performance and feedback to cope with problems as they occur.
Support and Feedback Mechanisms
During the early development phase, set up procedures for staff to flag and provide feedback. The 24/7 availability of support resources enables staff to immediately address technical issues and avoid downtime. It is through taking the patient feedback that valuable information for further developments appears and the system can be continuously made better to evolve.
Evaluate and Adjust as Needed
After the EMR system is up and running, it is important to carefully oversee its performance and impact on the clinic. Provide periodic surveillance and assessment of the system to determine if the system meets the goals established in the planning phase (i.e., whether the system’s purpose is to reduce administrative burden or improve patient care). It may be also required to make modifications to the system or additional training in order to make it more compatible with the changing needs of the user.
By performing these steps, it guarantees that your practice can smoothly move to an EMR system without, significant, disruption, allowing staff to transition seamlessly, while also improving patient care, and streamlining operations.
Conclusion
Implementation of an EMR system is a terminal step in the direction of health care practice modernizing, bettering patients’ care and automating processes. EMRs provide a suite of benefits ranging from better patient information management and administrative efficiency, through to improved care coordination using data analytics and actionable results on the ground. However, making the switch involves more than just software selection; it requires thoughtful planning, training, and ongoing support to ensure that the system truly meets the needs of both providers and patients.
Through the understanding of various categories of Hospital Management System and comparative analysis of its functions, cost, and expansibility, health care institutions can select a system that meets the current and future requirements.





