Introduction
What is a medical electronic record system?
A medical electronic record system, otherwise known as Electronic Health Record (EHR), is essentially a computerized copy of the paper chart that patients use to record their health. All basic medical information, including health history, medications, laboratory findings, physician notes, and so on, is available at one dealership. The purpose of this move was to facilitate data processing and retrieval within healthcare in such a way that now providers can have access to the right information faster, which would, in turn, help in support of more effective and better-connected care for their patients. How Does It Work?
The electronic storage and maintenance of the patient’s data in electronic form allows readily inputting, updating, and accessing patient documents by health professionals. EHRs tend to connect with those medical facilities so that registered individuals can access a medical history of a patient regardless of the location. So this way, interoperability enables better transition between health care settings and less use of paper, reducing medication and treatment errors.
By digital records retention, it preserves detailed and secured information as well as monitors. Quick access to health information, privacy of patients by compliance with guidelines, and assist with predictive analysis are also included. The medical electronic record system is a mode through which health trends are examined in clinical delivery as well as in the practice of patient care. It also boosts stock level quality, medication management, and inter-departmental communication.
Here we are, learning how EMR Software works, which advantages they add to healthcare professionals, managers, and patients, and why it transforms care delivery. We might see what new innovations in technology in the field will bring about more efficient and secure provision for all stakeholders.
What Constitutes an Electronic Health Record System?
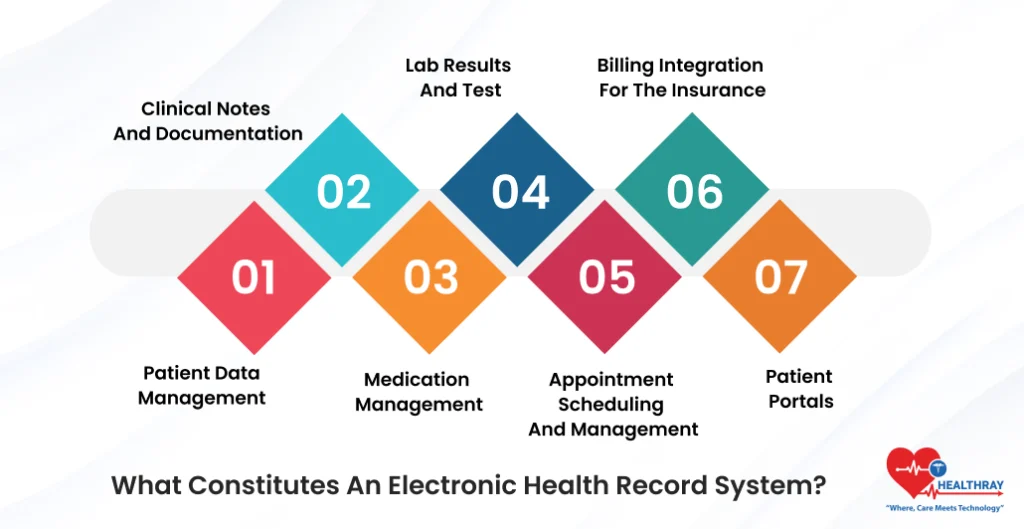
It is a combined mechanism that captures, organizes, and simplifies accessing patient data in a concerted effort to create a medical electronic record system, or EHR. Let’s take a glance at the most important components that make these systems functional and reliable:
Patient Data Management
This is the core outcome any EHR will derive; that patient data being collected will also include the patient’s name, age, address, and other particulars, as well as all medical history, made diagnoses, laboratory test results, findings, allergies, and immunizations. Such data will be taken down by the doctors or caregivers during each visit-further elaborating the entire picture for patients on their next visit.
With a proper medical record system, consolidation of bills and expenses for each patient becomes a set task. It is child’s play to transfer documents and medical reports between and among healthcare providers, speed up treatment planning and arrive faster than usual at decisions. Besides, patient stress regarding continuity in maintaining health records reduces. More so, it becomes easy for medical practitioners to write prescriptions.
Clinical Notes and Documentation
EHR allows a doctor and nurse to quickly document clinical notes. This takes observations, treatment plans, and progress notes. Such documentation becomes essential so as to streamline accurate ongoing care of the patient. For example, future providers can access the entire context of a patient’s treatment.
Medication Management
The area of medications prescribed does not include in its definition, and it has a record of prescription medication along with dosages and times. This module usually connects pharmacy information data; therefore, all drugs will be issued in a way that interaction is not established between between drugs.
Lab Results and Test
Patient results from other laboratory tests, as well as those from the radiological testing, are present in EHRs under which authorized personnel can access that data for immediate review. This situation accelerates decision-making processes, where response in the event that there would be changes in patient care mechanisms would be executed in time. In settings where rapid screening is required, access to Discounted Drug Tests can further support timely evaluations by providing cost-effective testing options without compromising reliability or accuracy.
Appointment Scheduling and Management
Several EHR systems have a scheduling module which helps to facilitate patients’ appointment and reminders which also reduces the no-show rates while optimizing patient flow and ensuring that providers have access to the correct records of patients prior to appointments.
Billing Integration for the Insurance
There is a coordination of insurance information along with EHR-supported billing modules. It eliminates billing errors, reduces the time taken in collecting payments, and keeps patients informed about costs and coverage as well.
Patient Portals
Other EHRs allow a patient to log himself or herself in a patient portal and view the patient’s health record, schedule an appointment, or message the health provider. Patient portals make accessing healthcare much easier and more accessible.
How EHR Systems Improve Patient Care and Healthcare Efficiency?

EHR systems deliver a number of revolutionary advantages at a healthcare process level and have greatly improved the ability to access information, coupled with better communication among providers. These very conditions are just a few of necessary features that could assure better care for the patient along with an efficient healthcare environment:
Improved Access to Information
Centralized medical databases of patients from EHRs can avail a complete medical record for a healthcare professional. This real-time access to patients’ medical histories, test results, and lists of medications makes it possible for doctors to quickly decide with much less complexity. This is important when timelines are of the essence, such as in an emergency situation.
Greater Integrated Care Coordination
EHRs make it possible to share information between different service providers. This means that the general practitioner, the specialist, and the surgeon have easy access to the file of the patient being discussed. Thus, care plans are organized, misunderstandings are eliminated, tests are not unnecessarily duplicated, and no medical errors are made.
Better Follow-Up Of the Status of Patients
Through the EHR, providers trace the time line of the follow-up of the patient. They follow patterns, track chronic conditions, compare previous data to the latest, which includes health information, and enable them to alter the treatments accordingly. This record will be most helpful among chronic patients for the proactive readjustment of their care plan.
Electronic Alerts and Reminders
Most EHRs use provider level alerting, which in turn provides an alert to practitioners regarding possible preventive screenings or drug-to-drug interactions. This self-initiated alert to the healthcare professional with regard to best practices and prevention of subsequent complications is very useful. For instance, alerting a doctor about the probable interaction between two drugs might help the patient avoid a serious health issue.
Reduces paperwork and administration stress
Manual records and paperwork are discouraged by the introduction of EHRs. This leaves enough time for the nurses, doctors, and clerks to care about people more than the search for records and filling out paperwork. Automated processes of billing, coding, and insurance claims take less time for administrative workflows to be completed without any glitches.
Informing the Patient Empowering
EHRs will enhance patient portals to become more participative with regard to health issues. This includes reviewing one’s medical record, treatment history, appointment information, and tests performed on him/her. Including doctors would cause a greater participation by patients.
Increased Safety and Compliance
EHRs increase protection for patient information through encryption and access control. This ensures that access by unauthorized personnel is limited, thus adhering to regulations, such as HIPAA in the US. Digital records will rarely go missing or in a misfile at facilities; therefore, maintaining accurate records.
EHRs thus improve access, coordination, and patient-provider engagement The resultant improved care is then translated into much better workflows. Hence, EHRs are managing to become an integral part of today’s health arena.
How EHR Systems Work Under The Hood – Healthray
Even though it’s easy to take for granted, the whole matrix of functions that EHR and EMR software provide is represented in these short words: accuracy, integrity, and availability of patient real-time data. Now let’s delve deeper into how these systems carry out a very efficient data management operation:
Data Collection and Data Entry
During the visit, the healthcare practitioner records the patient’s information alongside symptoms, diagnosis, medications, and test results. Some EHRs allow for voice recognition, so the providers may dictate their own notes, which has sped things up and minimized manual labor.
Data Storage and Management
This data is held in the system database using both cloud and on-site servers, granting good availability and security. The facility saves physical storage costs through cloud storage, while encrypted servers act against unauthorized access.
Data Integration and Interoperability
The software of EHR and EMR systems software operates with other health systems, such as lab information systems. It cooperates with pharmacy management platforms in this endeavor. This system updates lab results, prescriptions, and any other relevant information to ensure records are always current.
Secure Data Transfer
The encryption of data transfers is to ensure that patient information is sent to credentialed providers. The systems maintain HIPAA and other health standards; thus, they are sure that a patient’s information is kept private and can only be communicated with the provider.
Clinical Decision Support Ends
Many of these systems are supplied with clinical decision support features, such as alerts, reminders, and even evidence-based guidelines. This may be useful for therapy. For example, one may be alerted when an existing medication interacts with a new prescription, or a reminder may be set for preventive screenings for a particular patient.
Input of real-time data updates
The software of EMR Systems is designed in a real-time way to allow data to be accessed by whoever entered the information so that duplicate tests will not be done and conflicting treatments will not occur, and all the providers will work on updated information.
Audit Trail and Access Logging
There is the necessity to periodically check entries and alterations done on the patient file to remain compliant. Audit trails provide credibility whereby patients can be informed of unauthorized access traced to healthcare organizations with significant activities, thus providing assurance of patient trust and privacy.
Backup and Disaster Recovery
EHR and EMR are usually set up with the expectation of a backup and recovery procedure; they often backup to a secure server, thus, minimizing the loss of patient data through any technical failure and thereby continuing patient care.
In this scheme, that software operates within EHR and EMR systems protecting a bunch of data online; thereby reaching support in an appropriate case through various healthcare service-providing hands, and therefore information has been there in the real authentic systems all elevating patient care.
Benefits of EHRs

EHR systems, on the other hand, are tailored toward unique features for specified stakeholders in the health care sector: health care providers, hospital administrators, patients, and technology firms. This is how all of these benefit from the EHR systems:
Health Care Providers
For providers like physicians and nurses, and other health care professionals, with EHRs, care is now rendered more expedited through the contemporary access to accurate patient information.
Shifting from paperwork grants health care providers more time to interact with patients and deliver quality care.
EHRs provide real-time information on test values and patient history, which promotes expeditiousness in the processes of diagnosing and decision-making. In addition, clinical decision support tools including alerts about drug interaction ensure patient safety by minimizing chances of mistakes arising from administering the wrong treatment to patients.
Hospital Administrators
Productivity at the health facility is further enhanced since the EHR performs actual work rather than clerical duties.
Electronic systems have nigh eradicated hidden costs of paper documentation, while less storage space rises. Wallet-saving automated accounting and claims help in diminishing the paperwork and errors in the process of keeping clear financial records.
Analytical data are critical to administrators to predict trends in patient outcomes and, hence, facilitate streamlining of the practice operations for sounder choices on the use of resources.
Patients
EHRs empower the patients EHR systems allow for easy access for patients to medical records through use of patient portals.
They can view their histories, test results, and scheduled appointments for them-thus finding it easier in managing their health conditions. EHRs motivate patients to be concerned about their health journey through transparent access to their health record. EHRs help to eliminate duplicate tests and any corresponding delay in treatment; the patient receives timely and uniform care.
This ultimately leads to better coordination and interaction among providers with seamless communication with the patients.
Tech Companies and Innovators
EHRs represent numerous innovative opportunities for tech companies in the healthcare domain. The time is right for a change for many reasons, such as better data security, interoperability, and advanced analytics, the transition to greater user-friendly designs for EHRs in data sharing mode, and guarantee of data security.
When integrated with EHR systems, they will include AI, predictive analytics, and data integration. Innovations of this nature would turn into a real boon for either a healthcare provider or a patient. For instance, this organization would be fit enough to trigger a change in developing solutions around some very predominant pain points of the user interface-make it simple and take away cumbersome data input, and interfacing with other healthcare systems.
This indeed means better health care, supported by EHRs, which advocate for health care professionals’ convenience, help ease hospital management, and provide increased autonomy to patients. It is through EHRs’ integrated nature that all stakeholders become beneficiaries, thus facilitating an even more connected and effective healthcare ecosystem.
Future Trends and Innovations in EHR Systems
Technology endeavors continue to bring new developments concerning functionality upgrades, security, and user experience of the EHR system. Major trends shaping the future of EHRs are as follows:
Artificial Intelligence and Machine Learning
AI applied in the EHR eq. predictive analytics, decision-support, and personal-care recommendations. Then it would set off to machine learning algorithms allowing delving into prior patient data, picking up health trends to respond preventively even on the side of the provider. This is to say, AI, for physicians, would provide rapid and accurate insights toward a diagnosis to ensure better outcomes.
Improved Data Interoperability and Integration
The second problem in the health sector is EHR systems being unable to communicate amongst themselves. Interoperable data wholly shall be shared with complete fluidity between the health care system and health care facilities such that it allows one description of the patient’s history, accurately. This technology encourages the continual improvement in care and therefore reduces the risk of medical errors arising out of incomplete information.
For Security, Blockchain
This really makes EHR security by far the most decentralized storage, i.e., a safe unalterable ledger of patient records, resistant to unauthorized access of sensitive patient information for the life of that patient. Such technology, thus, allows for utmost patient autonomy over personal data by holding keys to allow/deny access to the data over a relevant, treatable period.
Mobility Access And Integration Of Telehealth
Mobile accessibility of EHR systems becomes a must as telehealth gains increased uptake. Most EHRs have consequently built new mobile-friendly interfaces that enable health care workers to access patient information on the go while they cannot access a computer or main EHR. Complementing this are the rising trends in favor of virtual consultations for better service delivery to these rural or short-on-resources areas.
NLP Technologies Ease Data Entry In EHR
NLP technologies improve EHR entry by transforming spoken words to structured text. With this enhancement, adding notes automatically removes the process from the list of activities to be done by health care providers, as typing the notes is time-consuming and increases the probability of error while making an entry in the data.
NLP, on the other hand, assists in retrieving relevant information otherwise hidden in unstructured data such as physician notes, patient discussions, and, generally enhancing the quality of EHR data.
Patient-Generated Health Data
Developments in wearables and in-home monitoring technologies are now also integrating with EHRs. PGHD offers assessment data against a realtime view of how the daily metrics affect patient data, horning in on heartbeat rate, blood sugar levels, or other indicators of physical exercise habits.
Further information serves to keep the providers on track in following the courses of chronic diseases and customize further adaptations for better treatment responses. Also, automatic gathering of this patient health data allows tracking even more to their health easily.
Advanced Analytics and Population Health Management
The trends were soon seen among large populations of patients who were to utilize the EHR as a resource for population health management. Through advanced analytics procedures, healthcare providers can track the patterns of chronic illnesses, identify outbreaks, predict them, or improve preventive strategies.
This presents an opportunity through which healthcare organizations can make available interventions which are indeed outcome-focused and thus improve community health on a macro scale.
All these forthcoming technologies and innovations are paving way for a more advanced, secure, and interconnected EHR system. Hence, as these trends develop, EHRs will more and more nourish quality patient care, lessen the administrative burden, and aid healthcare providers in taking more informed decisions in the shaping of the health future.
Conclusion
Medical electronic record systems or EHRs are transforming healthcare by centralizing patient information, lessening the administrative burden, and improving communication among providers.
Its integration with the hospital management system optimizes service delivery, as it interlinks all workflow operations in the facility. In that perspective, it has a ultimate role benefitting healthcare workers, administrators, and patients, from this point onwards allowing tech companies to lay the foundation for future systems. Trends now involve AI, blockchain security, mobile access, and all these attributes that make EHRs an important aid towards better patient care and effective healthcare delivery.
With greater enhancement in EHR technology underway, through hospital management systems, easing stakeholder health concerns and ultimately forming a cohesive view of a health organization for service delivery within an integrated and secure setting that reinforces the quality of care.





