The processes in the healthcare industry are constantly changing; one of the most important ones recently is the use of EMR systems. EMRs have changed the way patient data is handled in hospitals, clinics, and private practices in a way that is favorable in terms of care, efficiency, and patient safety.
In this EMR guide, we elaborate on everything related to EMR systems, how they help hospitals and healthcare providers, and the big hurdles. For owners of hospitals, clinics, and specialty doctors, an understanding of EMRs is of vital importance going forward in making proper decisions for your future.
How to Use the EMR System?
In an ideal world, the EMR system would allow you to funnel all sorts of patient or healthcare documentation. This documentation can either be in clinical documents or some other kind, like a prescription template, patient invoices, or appointment-related information. After filing documentation, access rights would allow you to access clinical information at one click.
Such consents would allow you to share with patients, providers, and any external specialists. Different procedures apply for IPD or OPD units. The EMR is also helpful for video consultations, claims management, and the billing cycle. Helping patients schedule appointments and obtain instant medical records and instant bill payment.
What Is an EMR System?
What Is An EMR System- Healthray
Thus, an electronic medical record is an electronic version of the patient chart, where any relevant clinical information like a diagnostic test result, medication, and/or treatment plan, progress notes, etc. could be electronically maintained for expedient access and, in turn, allow more accurate patient care through authorized access by health care providers.
These include a patient’s medical history, diagnosis, medications, treatment plans, immunization dates, and lab results. EMR records have advantages over paper records in that they are much easier to maintain and are prone to less human error.
EHR systems versus EMRs would be the next most important distinction. But despite being electronic records, they do not share the same commonality. The essence of the distinction is that EMRs differ from EHRs in that they limit interactive input by authorized health care providers, especially where multiple providers want to access a patient record, since an EHR grants such access.
Some Benefits of EMR Integration
Benefits of Integrating EMR Systems:
It brings the productivity up.
Paper records made simple the environment of coping with all the patient’s details. Unlike patient files intact maintained and updated, EMRs are fully information accessible for health providers to spend quite a lot of time. The access to patient information has been provided in real-time, nullifying any delay associated with those specific records.
It is connected to lab order, prescription, and billing systems so that work becomes quite fluid. Files will no longer wait in line during transfers between departments. 2. Quality of Care
Doctors have enough knowledge to make better decisions if they instantly have a complete medical history of their patients. Real-time treatment, drug, and laboratory data on patients are available through EMR, which could readily update alteration treatment plans. With this degree of accuracy, the risk of wrong decisions like drug prescriptions becomes minimized regarding the effects of other medications already taken by the patient.
Patient Safety
No medical error will be reduced as far as an EMR is concerned. Automated alerts for potential problems prompt those caretakers to take note of the significant interactions between drugs and possible allergies to critical lab values as well. This comes to make the omission or missing data, sometimes attributed to paper records, much less likely.
Because EMRs put reports together–test results, imaging, and clinical notes in one place–there is the very reduced chances of repeating tests or a failure to properly diagnose.
Data Accessibility
EMR systems grant privileged users access to information about patients anywhere. This is really large for hospitals that have different departments with many types of practices in different locations. No more shuffled paper records or waiting for another one to arrive from a department. Information is available at the click of a button.
It works in cases of extremes, where immediate access to the current patient’s information could make a difference between life and death in what care one decides to provide.
Cost Savings
While the investment for an EMR system is a pretty hefty price tag, the savings accrued in the long run are astronomical. It saves the cost of managing, storing, and retrieving paper records in veterinary practices. Costly medical errors and malpractice claims were minimized with EMRs which, in turn, advanced the whole efficiency in operations.
To add to this, streamlined processes in practices allow more patients to be seen in a very short period of time thereby generating more revenue.
Challenges of Implementing EMR
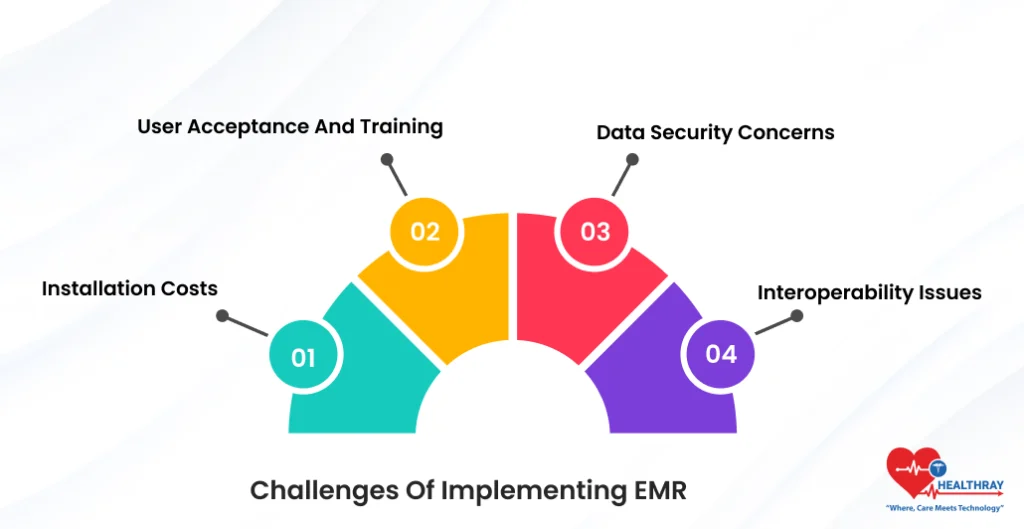
Installation Costs
Though EMR systems do save significant funds ultimately, the installation cost can pose an initial barrier. Software and hardware costs alongside the setting-up cost of the infrastructure, however, are one-time expenses, hard to digest by small-sized practices.
From that point psychologically, there would need to be considerations made about appraisal towards ongoing costs in maintenance, up-grades, and support.
User acceptance and training
This is a cultural change for the practice from paper-based documents to a computer-based system. Providers need to be trained to use the new system properly, which would create a short-term disruption to their normal work flows. Some who are older may resist because of feeling the way they have always done things has worked just fine for them, never having had to use a computer.
Training programs and vendor after-sales support can be instituted to avert the issues and smoothen the transition.
Data Security Concerns
There arise threats due to breaches and hacking because of sensitive patient information stored electronically. It is vital for the health provider to secure the data with robust systems such as encryption, access controls, and audit trails.
Ensuring compliance with data privacy regulation, such as HIPAA (Health Insurance Portability and Accountability Act), is important for protecting patient data and evading costly penalties.
Interoperability Issues
A correct EMR system should be interoperable with other systems of health care technologies such as laboratory systems, imaging systems, and even other EMRs. But unfortunately, very few among them posses interoperability to take on the burden of being integrated into existing health care infrastructure. This leaves data silos that disrupt the flow of information related to the care for the patient.
Criteria for Choosing the Best EMR System in Your Practice
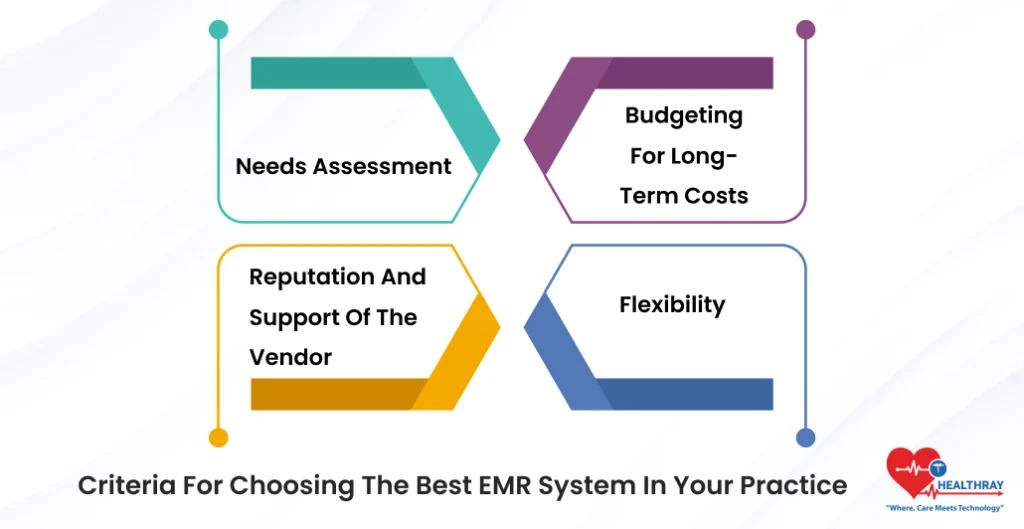
The Electronic Medical Records selection is one of the decisions that can really affect your practice for the years to come. Below are a few things you should consider when you are deciding:
Needs Assessment
Evaluation of the requirements of your practice: Start by evaluating the needs of your practice. Determine the size of your practice, how many patients it serves, and the flow processes that you would like to automate. Specialty practices might need EMR systems tailored to the unique documentation requirements of their specialties.
Reputation and support of the vendor
Pick a vendor with a clean history in health technology. An added bonus is a vendor who provides ongoing support in the form of education and troubleshooting to ensure that the installation runs smoothly. Just as you wouldn’t simply pick a brain injury lawyer randomly without regard for reputation and client outcomes, take time to examine customer reviews and feedback on the health care vendor. Therefore, the vendor should have an excellent reputation.
Budgeting for long-term costs
Admittedly, acquiring an EMR system has steep upfront costs, but there are running expenses that go toward updates, maintenance, and support. Even industries like brain injury lawyers emphasize long-term value when choosing digital tools, and similarly, you should consider an EMR system that remains affordable and sustainable for the long haul.
Flexibility
No practice is the same as the other, and hence it requires an EMR system that will positively support its workflows. You want to find that with-this-one-system-type-of-things-flexible-to-what-makes-your-practice-unique, without compromising the system’s functionality.
Conclusions
Certainly, so long as that EMR systems are said to promise efficiency and improved care with fewer errors, much is worth saying on the whole hijacked idea about revolutionizing healthcare practice by opting for the right system and properly implementing it regarding care-planned training and support. By knowing the various types of EMR systems and their advantages, hospital and clinic owners, as well as specialty doctors, will improve their decision-making process, which might then advance their practice in the years to come.