Medical coding is viewed across the healthcare industry as a tedious activity. Medical billing experts deal with anything ranging from coding to confusing insurance policies to popular mishaps concerning claims, all of which could increase delays to payment cycles and create some amount of administrative bottlenecks. Always, healthcare providers are searching for speed and accuracy in this process.
Enter: the AI-powered EMR billing system. It is ushering in a new era in how healthcare organizations carry out the billing process, completely automating repetitive tasks, minimizing errors, and speeding up claims processing. Fewer administrative hassles and better financial results will mean more time-both for hospitals, clinics, and billing companies.
The blog talks about transforming medical billing via advanced AI-enabled EMR billing systems. It covers all advantages it brings: the challenges it manages to sort out and everything else that might help decide if this is technology right for the organization. Stay tuned to learn about real use cases and the best one for your situation.
What Are AI-Based EMR Billing Systems?
At the most basic level, an AI-based EMR billing system comprises state-of-the-art technology with physical medical record management. Most fundamentally, the machines depend on artificial intelligence to fully automate billing into a more breezy, faster and more accurate process.
AI-enabled systems cut much of the manual input and repetitive jobs like traditional billing and automate as much of the work aspect as comfortably, allowing staff to concentrate on higher responsibility duties.
Here is how they work:
- Automated Data Processing: AI scans and processes the entire patient records so that correct billing codes are put in line with the services provided.
- Real-Time Error Delinquency Checking: These systems, when integrated, are able to find and flag discrepancies in claims or even documentation, which lessens the chances of rejection.
- Seamless EMRs Integration: Just as AI does with any other electronic medical record, it won’t double work but instead pulls data from existing ones to create right invoices.
- Predictive Analytics: With this, AI uses historical data to predict claim issues and suggests actions to be taken to avoid delay.
This entire automation speeds the billing cycle and reduces errors while leading to faster reimbursements and better financial returns for healthcare providers.
Clearly, the combination of artificial intelligence with EMR systems is more than a simple convenience upgrade-it is a strategic upgrade for healthcare organizations seeking to stay alive in such a fast-paced environment of medicine today.
Benefits of AI-Powered EMR Billing Systems

AI-powered EMR billing systems are built to address those common pain points in medical billing, be it reduced errors, expedited processes, or better revenue growth overall-these are all measurable improvements brought by these systems to health facilities.
The following analysis covers the important benefits:
Reduced Administrative Burden
Medical billing includes various repetitive tasks like claim submissions and follow-ups, or documentation. The responsibility of these mundane tasks would be placed into the hands of AI. Hence the staff would focus more on activities of higher value, such as patient care, or strategic planning.
Fewer Billing Errors
Claims have been denied, delayed, and regulatory affairs are mostly precipitated by erroneous medical billing. While making real-time analysis from data, AI identifies inconsistencies, automatically applying the correct coding. This allows for precise application, thus reducing the chances of rejections.
Expedited Claim Processing
Thanks to automation, the entire billing workflow is much quicker. From generating invoices to claim submission, every part of the whole billing procedure is reduced. Speedier processing means speedier refunds; cash flow could be managed effectively.
Better Management of Revenue Cycle
The claim-making procedure is optimized by AI-powered systems, which ensure that claims are specific and whole before submission. Additionally, their predictive capacities allow organizations to discern patterns in denials and advice on active steps to take to preemptively fix errors.
Cost Savings
Long-term savings outweigh the initial outlay for EMR systems powered by AI. Automation causes revenues to rise through reduced personnel needs in billing, lower error costs, and faster collection of revenue streams.
Enhanced Data Security
The security threatens the healthcare industry concerning issues like data breaches and compliance violations. Many of these AI systems come with built-in and, in many cases, very stringent security protocols so that patient data have been kept safe and in compliance with regulatory statements such as HIPAA.
Real-World Applications and Industry Leaders
Not just theoretical solutions, but AI-powered EMR billing systems are creating pathways in putting a premium on transforming most of the healthcare organizations worldwide. How exactly are these systems getting put to use, and which of these companies is probably blazing the trail?
Real-World Applications
In many ways, inefficiency in medical billing will be reduced by AI:
- Coding Assistance:
AI tools analyze medical documentation to attach the most appropriate billing codes to documentation, thereby achieving compliance and accuracy.
- Claims:
These systems check the lifecycle of claims from submission to payment, automatically identifying and correcting issues that would delay processing.
- Predictive insights:
Help to identify patterns in underpaid claims or missed opportunities for reimbursement, allowing providers to maximize revenue.
- Workflow:
AI automates mundane repetitive administrative tasks, thus reducing workload on billing teams and freeing them to concentrate on solving complex cases.
Examples of Industry Leaders
- Epic Systems:
Best known for their comprehensive EMR platform, Epic uses AI features in the billing systems to ensure billing accuracy and automates tedious repetitive processes. It aids organizations in proscriptive billing workflow while ensuring that coding standards are being looked after.
- eClinicalWorks:
The company has introduced conversational artificial intelligence, which would make EMR experience and billing much friendlier. Its system employs machine learning to recognize trends in billing and to help you get to actionable insights.
- Cerner Corporation: Cerner’s solutions powered by artificial intelligence weave automatic claims validation and real-time detection of errors in EMRs.
- Athenahealth: Targeted for the smaller practices, it utilizes AI to enable easier and efficient billing to avoid piling up of claims at the companies.
The Case Study Highlights
In a large cropland chain, an AI billing system was deployed, claiming frequent denial of claims. Six months later, denial rates fell by a significant 30%, while the billing cycle now hastened by 25%.
A mid-sized clinic adopted an AI application for coding assistance that resulted in premium productivity improvements by staff and decreased manual coding inaccuracies by more than 40%.
This sample is only one of many to show how healthcare providers and billing companies do not want to miss their chance in realizing the efficiency, cost-saving, and revenue-growing potentials that AI EMR billing systems have in store for them.
Challenges with the Introduction of AI in EMR Billing : Point
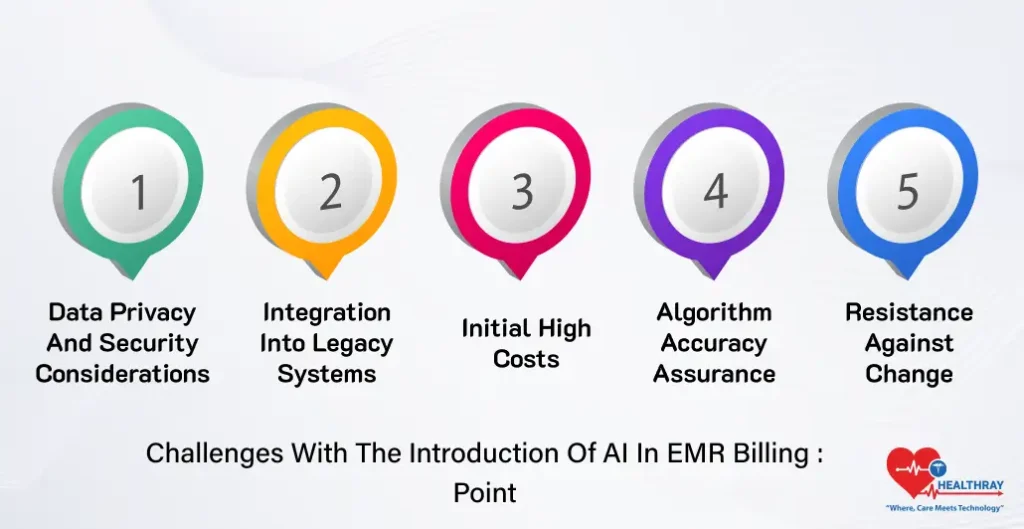
As much as they have advantages, so do the AI EMR billing systems bring challenges along with them during implementation. Understanding these hurdles would go a long way in smoothening the transition to optimal benefits from investments made.
Data Privacy and Security Considerations
The healthcare industry deals with sensitive patient data, making it a prime area for data privacy. AI systems that will be implemented would have to be HIPAA compliant and have stringent security measures, such as encryption and strict access controls. One lapse in these areas would lead to significant legal and financial consequences.
Integration Into Legacy Systems
Many hospitals already have legacy EMR platforms, many of which are incompatible with newer AI-enabled billing systems. The incorporation of AI into these systems can be tricky and generally requires custom solutions, resulting in higher costs and implementation time periods.
Initial High Costs
It is very costly to adopt AI-powered systems upfront because of all the investment in software acquisition, hardware, and training. These costs can deter smaller healthcare providers or billing companies from adopting the technology even if the expected returns exceed the initial investment costs.
Algorithm Accuracy Assurance
AI has its foundation in data. Inaccurate or incomplete data lead to incorrect billing codes, claims, and reports. Continuous monitoring and adjustment are necessary to secure the accuracy and reliability of these algorithms.
Resistance Against Change
Healthcare professionals may find new AI-powered systems intimidating because of the fear of endangering their employment or because they think it complicates their tasks. To overcome this fear, there should be encouragement through training and showing clarity on benefits.
Regular updating is part of keeping AI systems current and functional. This also consists of implementing updates to software in keeping with new regulations on billing or changes in coding standards. Without maintenance, the system does not fulfill its purpose of efficiency and precision.
Choosing AI EMR Billing Systems – Key Considerations for Choosing the Right System
Choosing an AI EMR billing system for your practice appears tedious as there are so many solutions out there at the moment. However, a rational approach will guarantee that the system selected fits seamlessly with your organization concerning its goals and operational needs. Some key pointers to consider while analyzing your options:
Growth of Your Organization
Healthcare organizations range in size from a small clinic to a huge hospital network. The ideal system must grow as one grows. For example, modestly sized practices may value simplicity more than a larger facility that may need advanced features such as predictive analytics or bulk processing.
Compatibility with Existing EMR Systems
One of the most important aspects of any adoption would be a concurrent integration. The existence of the billing system must be not based on the functionality of your current Electronic Medical Record platform and would not disturb the data flow. You should ask potential vendors about compatibility and whether they offer support for system customization, if required.
Security and Compliance
Data security is non-negotiable. Choose a system that adheres to industry regulations such as HIPAA and integrates robust data encryption, user authentication, and regular security updates. Make sure that the vendor has a proven track record of upholding compliance.
Customization and Automation Possibilities
Inquire whether this system has these features and how much latitude it gives users to customize automation according to their preference. For example, auto-coding and real-time error detection are essential aspects when transactional claims are considered because they offer protection against claims with possible manual errors. Customization options should also be available to tailor to your organization’s workflows.
Vendor Reputation and Support
Always substantiate vendors thoroughly. Well-noted vendors with experience in health AI are worth checking into. In addition, a reputable vendor makes sure to render support and training so that its clients’ systems continue to operate smoothly.
Cost and Return on Investment
Letting the initial price as well as potential future worth weigh on your decision-making. More sophisticated systems will generally have a higher initial cost upon installation, yet there are greater chances of billing accuracy and lower claim denial with quicker process calls for good onward ROI.
Proper Training and Ease To Use
Without proper training, even the most sophisticated system will become a liability. Opt for a vendor who offers comprehensive staff training and on-the-job training. The interface should be user-friendly to negate excessive amounts of learning curve challenges.
The Point on the Future of AI in Medical Billing
The value of AI for medical billing is constantly changing. At the same time, its promise is still not fully manifest. Combined with inventive applications, state-of-the-art emerging technologies are expected to transform the way healthcare institutions will bill, claim, and manage finances in the future.
Enhanced Predictive Analysis
AI would create employable predictive models to preempt trends likely to increase in the future of billing and claims processing. For example, systems would detect patterns in claim denial, which prevention measures would be directly implemented.
This prediction might further enable healthcare practitioners to really gain optimization in revenue cycle management.
Automated Revenue Cycles End-to-End
Full automation is expected from AI systems in the future, where processes handle the full cycle of billing-from the initial data collection about the patient until developing a claims submission with follow-ups-all with no intervention from human beings. This will save a great deal of time and cost in terms of operations.
Improved Patient Transparency
AI-enabled systems will adequately address patients about their bills and terms of billing. Through natural language processing (NLP), they can establish well-understood, patient-oriented invoices and reply to frequent queries on billing, thus reducing confusion for patients and increasing satisfaction.
Better Fraud Detection
AI has long been used to detect anomalies in billing data; however, strides in the future promise to enhance fraud detection capabilities significantly. The systems are now able to not only identify irregularities, but also identify possible fraud in real time, thereby protecting both the providers and patients.
Personalized Billing Solutions
Using machine learning, AI can automatically design personalized billing plans depending on the financial profile of a patient and his or her payment capacity. This move would probably increase collections and be patient-friendly.
Integration with the Wider Healthcare AI Ecosystem
AI in medical billing will not operate in isolation; rather, it will involve all other AI-based systems in healthcare-a totality of diagnostics, management of patient experience, and so on. In short, the world will make all operations streamlined.
Conclusion
As systems are developed around EMR billing, AI in hospitals will now be transforming the face of billing in these healthcare organizations in making billing processes more effective. It will bring distinct kinds of efficiency, removing time-consuming repetitive processes, eliminating errors, and refining revenue cycles. Such tools for hospital administrators, healthcare providers, medical billing companies, and IT professionals are not just making billing better. They are designing a more efficient and patient-centric healthcare experience.
Yes, there are problems: integration, data privacy, and other such issues. But the gains will far outweigh the costs. Organizations that embrace the right system will quickly and effectively reduce costs and time in preparation for an increasingly precision-demanding industry.
In fact, now is the time to take the first step in transforming medical billing with artificial intelligence. The future of billing is here today, and it is powered by AI.




