Efficiency and effectiveness are the key concerns of healthcare in the modern environment. EHR software is not only a tool for data storage but also a powerful means to enhance patient safety and simplify the work of healthcare professionals. EHRs changed the way patient information is utilized by health professionals. From reducing medication errors to their history being accessible anywhere, EHRs are one of the cornerstones in providing patients with the safest and most effective treatment possible. This paper analyzes the key benefits of EHRs to patients’ care and how EHRs ensure patient safety for improved health outcomes.
Key Benefits of EHRs to Patient’s Care
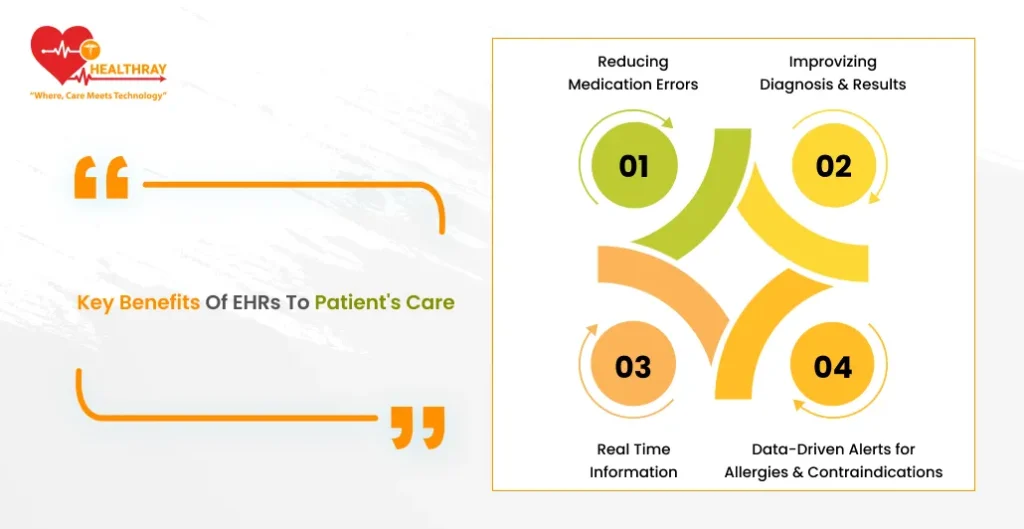
Reducing Medication Errors
EHRs make a difference in patient care in many ways, including the reduction of medication-related errors. A hospital or clinic environment is intensive with work and may sometimes be careless; even a minor mistake can have disastrous consequences. EHR Software is designed to mitigate such risks by offering inbuilt safety features that include medication reconciliation and drug interaction alerts.
These systems can also automatically flag possible dangerous interactions with prescribed medications or patient allergies. For example, if a physician tries to prescribe a drug that may cause a severe reaction, based on the patient’s allergies, the system automatically notifies the doctor and such prescription is therefore not processed.
EHR removes the game of ginnies or blind man’s buff in drug prescription which goes along the way of really improving safety for a patient. EHRs provide all medicines histories of the patients, that form the important bases while caring for these complex needy individuals.
Improvizing Diagnosis and Results
Due to EHRs, healthcare providers will instantly have access to a patient’s complete medical history. This would lead to quicker and more accurate diagnoses, and proper treatment could be given based on the comprehensive view of a patient’s condition that doctors will have.
It would help, for example, when a patient has chronic illnesses such as diabetes or heart disease; the history of treatments and their results in terms of lab and imaging studies lets the healthcare provider undertake the best course of action without undue repeat tests. This saves not only time but also health resources and improves outcomes in patients.
Moreover, EHRs lay the structural groundwork for pooling together data from other places through which doctors could get patterns on how to address and treat patient care that, if not documented through EHRs, will pass without the doctors identifying them.They help provide better coordination of care among caregivers.
In modern health care, and especially in the hospital environment, one patient sees many providers. EHRs ensure that the same real-time data is accessed by all the care providers from specialists down to the nurses, facilitating easier coordination of care across departments.
Without EHRs, information is often lost in translation across departments, either in the form of duplicated effort or critical oversights.
A patient referred by a primary care physician to a specialist immediately has a full medical record accessible and thus continuity of care with no delay. This level of coordination especially requires patients that have a chronic illness or those often transferring between a care setting. EHR allows all parties’ seamless communication regarding the patient reducing errors along with making sure results.
Real Time Information
Every minute counts in an emergency. Full access to the patient’s record can be the difference between life and death. EHRs enable healthcare providers to retrieve vital information about the patient instantly, even in time-sensitive situations.
For example, if an unconscious patient is admitted to the emergency room, medical professionals can easily access the patient’s medical history, such as allergies, previous diagnoses, and medications. This helps doctors to avoid harmful treatments for the patient and do their best to treat the patient based on the information at hand.
Data-Driven Alerts for Allergies and Contraindications
The alert systems in EHRs flag providers regarding risks for allergies or drug contraindications, acting as an added layer of protection to avoid missing important information.
For example, if a patient is allergic to penicillin, the EHR system would immediately flag this the very moment it is prescribed by any physician. Such alertness averts the possibility of medical mistakes that may lead to serious consequences or even death. Besides medication alerts, EHRs are able to flag contraindications in potential treatment plans. This makes certain that healthcare providers make appropriate decisions based on considerations that are appropriate and safe for the patient.
The Role of EHRs in Population Health Management

While EHRs help the individual patient, they also have a massive role in enhancing the outcomes of public health because such records allow healthcare providers to better manage population health.
Monitoring and Managing Chronic Diseases
EHRs enable tracking and monitoring of chronic diseases on the part of health care providers more effectively. Aggregating population-level data allows health care providers to identify patients who are at risk for complications and thus provide proactive interventions. For instance, through the EHR system, a clinic will be able to treat patients that have diabetic conditions, monitor the level of blood sugar, and tell whether the patients get screened on time. Through the monitoring of these indexes, health care providers can give more specific care and intercept the emergence of problems before they progress into further steps.
Public Health Insights
EHRs can also allow health professionals to obtain data they will later analyze and thereby use as public health intervention. For instance, through the EHR, health care providers could utilize this aspect in vaccine uptake and trace who misses certain vaccinations that will need direct intervention. Data obtained this way could also be used in the making of follow-up statistics shared between health care services and public agencies regarding the spread and direction of diseases’ patterns in relation to changes in any particular health trends.
Managing Implementations of EHRs
Moving Beyond the Inherent Benefits Despite the proven benefits of an EHR implementation, it isn’t without overcoming some challenges: cost, training, or workflow disruptions from the organization part to be addressed during the implementation.
Usability-Related Issues
Usability is one of the major challenges toward EHR implementation. EHR systems in healthcare can be very complex for health care providers, especially those working with paper-based systems, to navigate through; however, proper training and ongoing support can help avoid these issues.
Healthcare organizations can also help by providing training programs that will make all staff comfortable in using the system. Also, most vendors providing EHRs now offer friendly interfaces where entry and retrieval of data are less cumbersome.
Cost and Workflow Adjustments
The cost of implementing an EHR system is very high and quite unaffordable for small clinics. But this should be treated as a long-term solution that will increase efficiency and lower operational costs in the long run. EHR systems do require some changes to the existing workflows. For example, health providers may take more time to do things while learning the new system. With time, however, the system will be fine-tuned: less paperwork and better patient care, with accuracy and efficiency.
Conclusion
EHRs are way beyond a simple organizational tool in managing patient information; they form a critical part of modern healthcare systems, actually working toward improving patient safety and outcomes. Long-term benefits, ranging from reduced errors to improvements in care coordination and population health management, will result for both the provider and the patient with EHRs. For the owners of both hospitals and clinics and doctors in all specialties, investment in EHRs will give them a better chance to be competitive in today’s healthcare setting. As it may have initial costs and an introduction period, the advantages far outweigh disadvantages. EHRs improve patient care while delivering health services more efficiently.